Chiropractor, Dr. Alexander Jimenez details the relevant anatomy and biomechanics of the hamstring, common mechanisms of injury, the clinical signs and symptoms and management in the kind of surgical repair.
Introduction
Hamstring injuries in athletes are re-injury and typical to the hamstring is a reasonably frequent occurrence. Orchard and Seward (2002) found that at elite-level Australian Rules football, hamstring injuries were the most common kind of injury requiring time off from competition. Muscle strains are the most frequent, followed by more significant myotendinous junction tears. These respond well to rehab. Total ruptures of the muscle are uncommon as are complete ruptures of the hamstring origin (Steinbruck 1987), and accidents like these can be very painful.Hamstring muscle origin ruptures in the kind of avulsions of the growth plate are more frequent in younger populations due to the immature epiphyseal growth plate (apophysis) found to the ischial tuberosity in older children and adolescents (Wootton et al 1990). Avulsions in adults with ischial tuberosities that are fully-fused have a tendency to be ruptures of the proximal hamstring tendon or complete avulsion fractures of the ischial tuberosity.
Prompt diagnosis and proper treatment of ischial tuberosity avulsions/ tendon ruptures is critical due to the residual loss of power persistent in non-operatively treated instances of hamstring ruptures (Birmingham et al 2011). The ongoing complications with chronic non-repaired complete hamstring tendon avulsions are pain, weakness and cramping during locomotion and pain with sitting (Wood et al 2008, Harris et al 2001). As with most tendon avulsions repair leads than delayed repair. Repair within four weeks of injury resulted in better outcome compared with those repaired after four weeks (Harris et al 2011)
Relevant Anatomy & Biomechanics
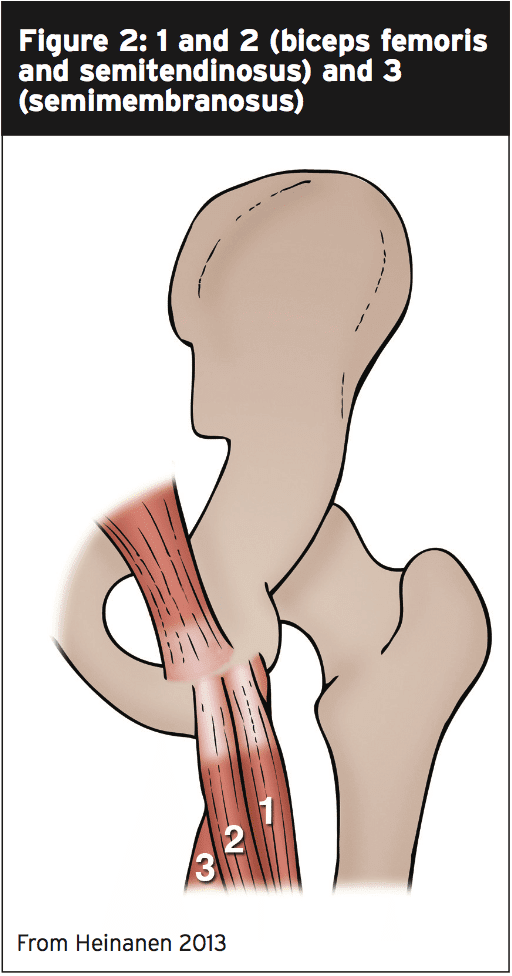
The hamstring muscles comprise the biceps femoris (long head and short head), semitendinosus and semimembranosus. All muscles (except biceps short head) attach onto the ischial tuberosity. The head biceps starts on the femur along the linea aspera.At the origin, the head attach to the ischial tuberosity and of the semitendinosus and bicep form a conjoined tendon and the semimembranosus with its tendon attaches. Figure 2 shows the attachments of the two individual heads.
At puberty there appears at the ischial tuberosity a secondary ossification centre and this doesn’t fuse until the late teens or early twenties. In this time frame between the appearance of the apophysis and its fusion, a force traction on the hamstring may avulse the apophysis as this forms the weak link between the muscle and the bone. After skeletal maturity, injury is more likely to take place at the junction.
The hamstring origin is intimately connected to the sciatic nerve’s passage during the upper posterior thigh. Serious injury to the muscle that produces a large hematoma may create adhesions in the vicinity of the sciatic nerve that may complicate the athlete’s performance when recovered, or the nerve may be injured due to a grip neuritis as the muscle belly retracts away from the nerve (Chakravarthy et al 2005) or due to compression from a tight fibrotic band directly to the ischial tuberosity. Diligent treatment of sciatic nerve mobility is a significant element in hamstring rupture direction (see below in conversation on management).
It is not unusual for the hamstring origin rupture to involve only two heads of not all three and the hamstring. These are classified as partial avulsions. It is more common if the avulsion is partial that it involves the conjoined tendon of the biceps femoris and semitendinosis (Heinamen 2013).
Mechanism Of Injury (MOI)
The hamstrings are vulnerable to trauma due to the anatomical arrangement and on account of the leverage that acts through the hip during functional movements.The most frequent MOI is forced knee extension in a position of hip flexion and as the muscle is placed below a rapid and large eccentric load. The force is directed to the junction. This is sometimes due to a sudden and forceful landing from a jump with the knee locked in extension, or during foot contact in sprinting, or in excessive and uncontrolled hip flexion such as when the leg slips out from underneath the body and moves into hip flexion with the knee extended (forward splits, water skiing and bull riding).
However, it is thought that in order for tendons to rupture, a degree of degenerative change needs to be present in the tendon prior to rupture. This has been observed that rupture and supraspinatus tendons that rupture. This possible clarifies why myotendinous ruptures in the hamstrings of young athletes almost never happens, they fail at the growth plate and might also explain the rising frequency at middle aged recreational athletes (Cohen and Bradley 2007).
Signs & Symptoms
The usual mechanism of injury has been described above, and the pain can be severe and debilitating once the hamstring origin ruptures. The athlete describes it as ‘being shot by a sniper’. An audible ‘pop’ may be heard. The athlete will be guarded on the affected limb and will be reluctant to weight bear on a loaded limb.On examination, a palpable defect may be felt below the ischial tuberosity and a loss of the contour of the hamstring may be observed, however these will be dependent on the size of the gluteals and any intervening adipose tissue that may make direct palpation and visualization difficult. A discolouration may be seen throughout the muscle, if the athlete is examined following the incident.
The athlete will demonstrate a painful weakness in both knee flexion and hip extension that is isolated. Range of motion is going to be as they’ll be unwilling to weight bear pain functionally and restricted they may walk with a limp.
Presentation to the practice has been delayed, generally because the athlete assumes the injury is purely muscle-related and will heal, if, then the patient may show atrophy of the hamstring muscle due to disuse.
Imaging
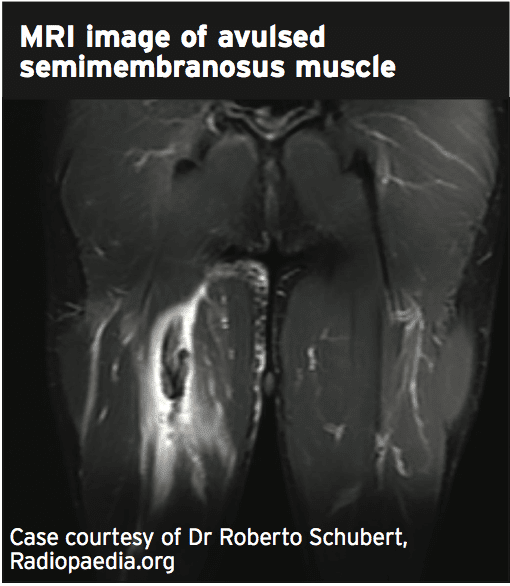
CT imaging and plain x-rays supply little use unless an avulsion of the hamstring tendon from the ischial tuberosity has happened.Ultrasound imaging may be helpful; however, its sensitivity and specificity has not yet been reported.
As the delicate tissue detail is visualized in an MRI, MRI is the investigation of choice in a suspected rectal origin rupture and it can highlight tendon retraction’s level in addition to any interference with the nerve. Furthermore, MRI can be used in through all phases of recovery to appraise the therapeutic capacity of the tendon.
Management
The treatment of hamstring origin injuries is contentious; fix or not fix. A number of standards have been suggested that can help the practitioner decide if the hamstring injury requires surgery (Domb et al 2013):1. Osseous avulsion with more than 2cm retraction;
2. Complete tears in all 3 tendons with or without retraction;
3. Partial tears that remain symptomatic despite prolonged conservative treatment.
However, some and complete incomplete ruptures of the hamstring origin will require treatment in the vast majority of athletes on account of the concerns regarding loss of strength and power.
The case for operative management of partial hamstring origin rupture is not as clear-cut. It may be that some of these can rehabilitate well following a partial rupture; however, if pain and dysfunction persist after a lengthy rehabilitation process, then repair of a partial rupture can result in good clinical outcomes (Aldridge et al 2012). However, Lempainen et al (2006) presented a series of partial hamstring ruptures that responded well to surgical intervention.
Surgery
The hamstring is approached with a posterior incision starting at the gluteal fold. The incision may extend over a distance to completely access the hamstring tendon that is retracted. The posterior cutaneous nerve and the sciatic nerve is going to be visualized and any adhesions can carefully be resected (neurolysis). A neurolysis will be necessary if the surgery was delayed due to failure or a delayed surgery following treatment. This will be evacuated, if there is a hematoma observed.The proximal tendon stump on the ischial tuberosity will be found as will the retracted tendon and these will be approximated with the knee in flexion (to decrease the hamstring stretch). They will be repaired with Ethibond sutures and Merselene tapes. This will be anchored tapping screw if the tendon has avulsed of the tuberosity.
By flexing the knee to 45 degrees to create tension the integrity of the repair will be tested. This enables the surgeon to check the ‘safe’ available range of motion intra- operatively so that physiotherapy can start early (at two weeks) in the safe ranges. This will avoid a prolonged immobilisation that’s been demonstrated to lead to range and strength loss and significant atrophy in hamstring repairs.
Then the demand for a postoperative knee flexion brace is not required, if the injury is reasonably new. However, if the surgery was delayed due to failed conservative management a knee flexion brace post-operative may be required.
Some authors have attempted endoscopic repair of the hamstring tendon and state that this procedure offers more benefits like minimal scar tissue, superior visualisation of the hamstring tendon, decreased bleeding and better protection of the neurovascular bundle (Domb et al 2013).
Post-Surgical Outcomes
Almost all studies conducted on the outcomes of hamstring tendon repair in return and strength return to function show that it is unreasonable to expect that the athlete returns to full strength in the hamstring following a hamstring tendon. Although the strength of the hamstring is still diminished, the athlete can return typically to a pre-injury amount of competition.Wood et al (2008) found that in those with repaired hamstring tendons, 80% returned to pre-injury heights of sports. What’s more, hamstring strength returned to a level of 89% to a mean of 84% and hamstring endurance. Konan and Haddad (2010) found that 90% of the hamstring injuries they tracked returned to pre-injury levels of sport. Isokinetic testing and all reported functional outcome showed that the hamstring strength returned to 83% at six months compared with 56% at the pre-surgery level. Finally, Cohen and Bradley (2007) reported on seven patients who underwent operative repair and found that average time to return to function (and sports) was 8.5 months. To pre-operative levels of function, six of the seven had returned by post-operative six months.
References
- Aldridge, S.E., Heilpern, G.N., Carmichael, J.R., Sprowson, A.P., Wood, D.G. Incomplete avulsion of the proximal insertion of the hamstring: outcome two years following surgical repair. Journal of Bone and Joint Surgery. 2012. 94(5); p. 660-662.
- Birmingham, P., Muller, M., Wickiewicz, T., Cavanaugh, J., Rodeo, S., Warren, R. Functional outcome after repair of proximal hamstring avulsions. The Journal of Bone and Joint Surgery. 2001. 93-A(19):p. 1819-1826.
- Chakravarthy, J., Ramisetty, N., Pimpalnerker, A., Mohtadi, N. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a case report of four cases and review of the literature. British Journal of Sports Medicine. 2005. 39; p. 569-572.
- Cohen, S., Bradley, J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007. 15(6); p. 350-355.
- Docking, S., Samiric, T., Scase, E. Purdham, C. Cook, J. Relationship between compressive loading and ECM changes in tendons. Muscle Ligaments Tendons J. 2013. 3(1); p. 7-11
- Domb, B.G., Linder, D., Sharp, K.G., Sadik, A., Gerhardt, M.B. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech. 2013. 2(1); p. e35-e39.
- Harris, J.D., Griesser, M.J., Best, T.M., Ellis, T.J. Treatment of proximal hamstring ruptures: a systematic review. Int Journal of Sports Med. 2011. 32(7); p. 390-495.
- Heinanen, M. Proximal Hamstring Avulsion – Anatomy, Cause of Injury, Surgical treatment and Post-operative Treatment Protocol. Suomen Ortopedia ja Traumatologia. 2013. 36: p. 104-110.
- Konan S, Haddad F. Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010; 34:119-23.
- Lempainen, L., Sarimo, J., Heikkila, J., Mattila, K., Orava, S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. British Journal of Sports Medicine. 2006. 40; p. 688-691.
- Orchard, J. and Seward, H. Epidemiology of injuries in the Australian Football League, seasons 1997–2000. British Journal of Sports Medicine, 2002. 36; p. 39-45.
- Pombo, M., Bradley, J.P. Proximal hamstring avulsion injuries: A technique note on surgical repairs. Sports Health. 2009. 1(3); p. 261-264.
- Steinbruck, K. Epidemiologie von Sportverlezungen. 15-Jahres-Analyse einer Sportsmedizinischen Ambulanz. SportsvertetzSportsch, 1987. 1; p. 2-12.
- Wood, D.G., Packham, I., Trikha, S.P., Linklater, J. Avulsion of the proximal hamstring origin. Journal of Bone Joint Surgery (Am), 2008. 90-A; p. 2365-2374
- Wootton J.R., Cross, M.J., Holt, K.W.G. Avulsionof the ischial apophysis. The case for open reduction and internal fixation. Journal of Bone and Joint Surgery. 1990. 72; p. 625-627