Science based chiropractor, Dr. Alexander Jimenez looks at frequent mechanical causes of heel pain -- and how they can be seen and treated.
Plantar heel pain is a frequent presentation to sports clinicians and might be result of mechanical, neurologic, traumatic or other systemic illnesses(9). Plantar fasciitis is undoubtedly the most common pathology in this area seen by cliniciansnonetheless, other causes of heel pain has to be considered when assessing a customer with heel pain. Up to two million Americans report heel discomfort each year at a price estimated to be up to $400million(5). Despite this, little is known about the pathophysiology and etiology of plantar heel pain. This article will discuss plantar fasciitis in addition to other frequent mechanical causes of heel pain such as plantar fascia tears/rupture, heel pain of neurological source, calcaneal stress fracture and atrophy of the heel pad. The anatomy of each of those illnesses will be discussed as well as diagnostic criteria and potential treatment choices will be summarized.
Plantar Fasciitis
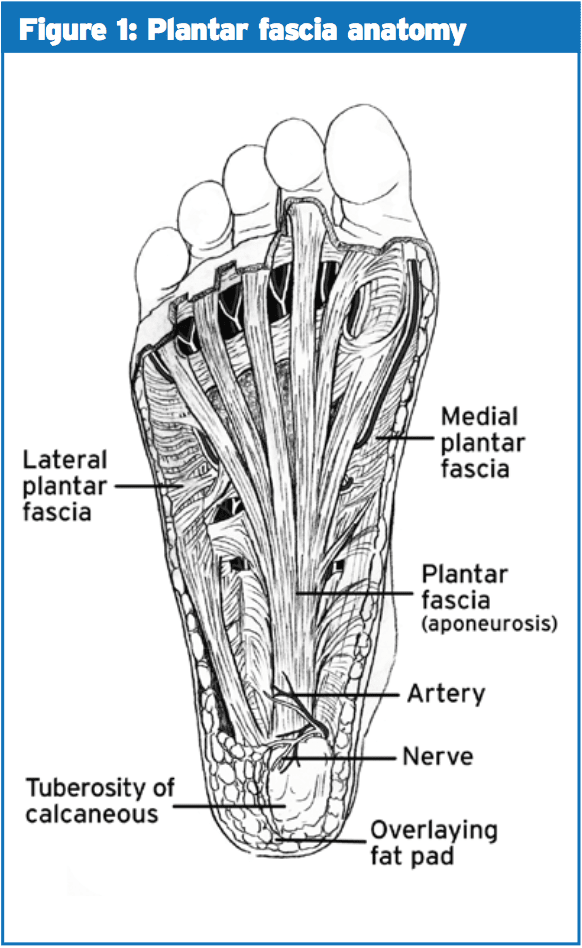
The plantar fascia is fibrous aponeurosis that spans from the calcaneal tuberosity to the proximal phalanges(6) (see Figure 1). Plantar fasciitis most commonly occurs by mechanical disturbances because of either bio- mechanical flaws, obesity or work habits(10).
Assessment & Diagnosis
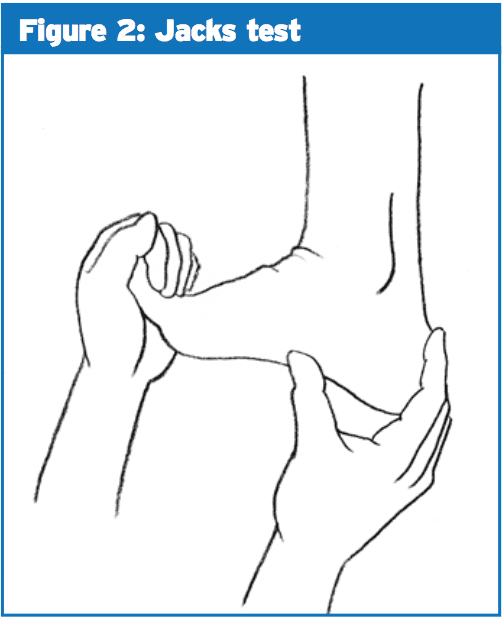
Patients presenting with plantar fasciitis most often complain of pain on the first few steps in the morning when getting out of bed or after prolonged rest(2). This has been termed "post- static dyskinesia"(2). Maximal tenderness is over the origin of the plantar fascia on the medial calcaneal tuberosity(2). Jack’s test, which involves passive extension of the first MTP joint, tests the integrity of the plantar fascia and the Windlass mechanism (see Figure 2).This could include but should not be limited to:
- midtarsal, subtalar and ankle ROM
- calf flexibility
- gait assessment
- footwear inspection.
1) fascial thickening greater than 4-5mm,
2) deceased echogenicity,
3) perifascial effusion may occasionally be seen(4).
2) deceased echogenicity,
3) perifascial effusion may occasionally be seen(4).
An infra-calcaneal spur might be present but these also have been observed in asymptomatic individuals also, and elimination of the spur doesn't appear to add to the achievement of plantar heel pain surgery(10).
Treatment
The Heel Pain Committee of the American College of Foot and Ankle surgeons, based on available evidence in 2010, determined three tiers of treatment modalities for plantar fasciitis(10).They said that Tier 1 treatment options must be trialled first, which include:
- padding and strapping of foot
- stretching exercises of calf and foot
- home cryotherapy
- avoidance of barefoot or flat shoes
- over-the-counter arch supports/heel cup
- oral anti-inflammtories
- corticosteroid injection
- weight loss.
- night splints
- further injections
- immobilization
- prescription orthotics.
Traditionally corticosteroid has been the injection of choice with respect to plantar fasciitis; however, some evidence points to short-term relief only. As well as poor long-term effects, other risk factors related to corticosteroid injection (CSI) such as fat pad atrophy, osteomyleitis of the calcaneus and iatrongenic rupture have all been reported(2). Platelet rich plasma (PRP), which is a concentration of platelets derived from the plasma part of autologous blood (like growth factors), has also been trialled as a treatment option for plantar fasciitis. Aksahin compared CSI and PRP and reported comparable results at three months and six months (approx 50% drop in VAS scores) also claimed that contemplating the risk factors related to CSI PRP might be a better alternative option(1). Diaz-Llopis compared botulinum toxin type A (botox) with CSI and revealed that the botox group was slightly better at one month but considerably better than the CSI team at both six and twelve months(7,8). Additional research has to be conducted on which injection modality gets the best results over both the short and long term.
Plantar Fascia Tears/Rupture
Intense strains of the plantar fascia occur quite frequently and normally, should they happen in isolation, react relatively quickly to treatment. They may be associated with plantar fasciitis, particularly if a CSI was trialled. Clients with an acute tear describe a sudden beginning heel pain and may have localized tenderness over the plantar fascia, along with a palpable lump might be present in case a partial or total rupture is present(4). In the case of significant tears that they are going to have pain on weight bearing. Treatment is symptomatic and involves initially a non-weight posture boot and innovative weight bearing with inviting taping and/or orthotics as pain allows.Heel Pain Of Neural Origin
Up to 15-20 percent of individuals with plantar heel pain is brought on by entrapment of branches of the tibial nerve(2). This nerve can get entrapped in the possible sites:
1) where the nerve passes at the sharp edge of the abductor hallicus;
2) just distal to the medial edge of the calcaneus;
3) due to compression between the abductor hallicus and the quadrates plantae muscles.
2) just distal to the medial edge of the calcaneus;
3) due to compression between the abductor hallicus and the quadrates plantae muscles.
The second most frequent cause of heel pain of neural origin is entrapment of the medial calcaneal nerve which innervates the heel fat pad and superficial tissues overlying the inferior calcaneum(two). Most branches of the nerve lie superficial to the intrinsic muscles of the foot so it is less likely to be compressed within these muscles, but might be compressed or irritated following heel pad atrophy(2).
Assessment & Diagnosis
Much like plantar fasciitis, their pain is most often worse after intervals of rest but might also occur at rest and at non-weight bearing positions. Although paraesthesia or anesthesia is infrequent, it may be reported around the medial or plantar surfaces of the heel(2).On physical examination, nerve entrapment should be suspected if the site of maximum tenderness is over the nerve.
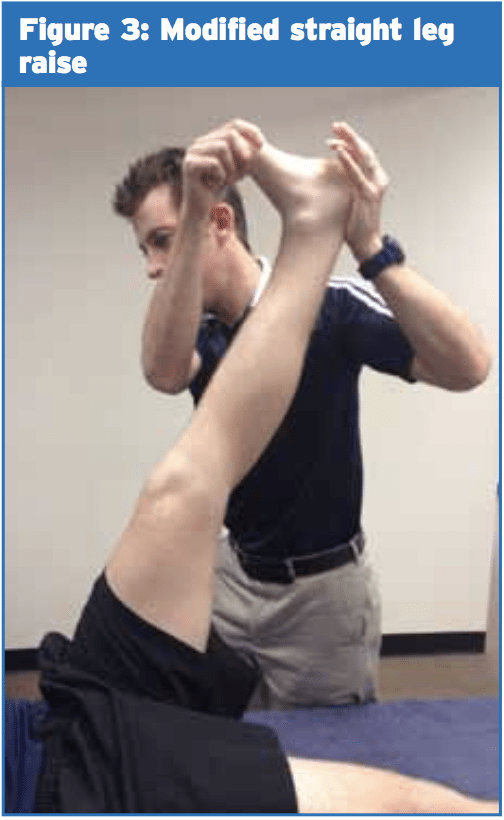
Neurodynamic testing may play a part in the identification of nerve involvement of plantar heel pain. Altered straight-leg increase testing that additional dorsiflexion, eversion and toe extension increased strain on the tibial nerve and LPN and when hip flexion was inserted no additional load on the plantar fascia has been noted(2). Differentiation of the plantar fascia as well as the tibial nerve may be carried out with the addition of hip flexion. Figure 3 shows the modified SLR for the tibial nerve and its branches.
Treatment
Despite its various pathophysiology and etiology, current study suggests the treatment of plantar heel pain of neurological source should be similar to that for plantar fasciitis. This absence of specific treatment options for your differing presentations may be among the reasons why plantar heel pain may be so recalcitrant. It could be suggested, like nerve entrapments in different parts of the body, "port" function and nerve gliding or sliding exercises may be useful to cure and prevent ongoing entrapment. Further studies need to be done in order to determine the most effective treatment for all these neural entrapment syndromes of the foot.Fat Pad Atrophy/Contusion
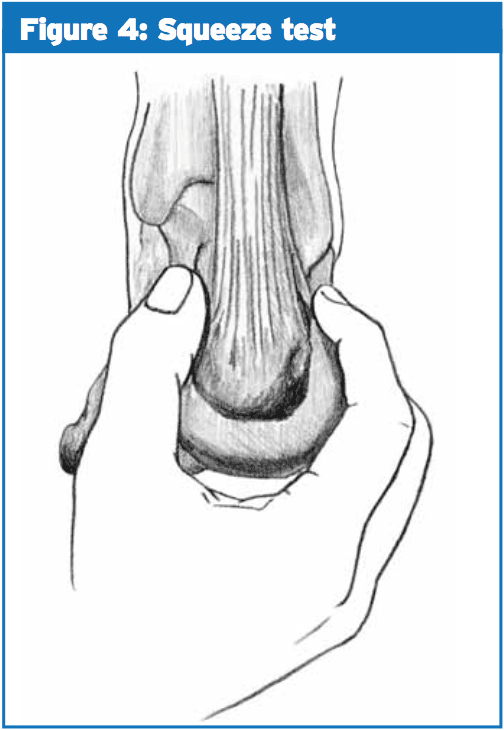
The calacaneal fat mat comprised of elastic fibrous tissue and carefully packed fat cells that act as a shock absorber on heel strike(4). This problem is often related to plantar fasciitis but can be an isolated thing. Patients with fat pad atrophy may report pain aggravated with walking particularly in hard shoes or on hard surfaces(4). Commonly due to the heel strike pattern, pain is felt more over the lateral aspect of the heel that helps to differentiate it from plantar fasciitis.Stress fractures of the calcaneum are quite common and mainly occur at the upper posterior margin of the os calcis or adjacent to the medial calcaneal tuberosity(4). Patients with a calcaneal stress fracture will report insidious onset heel pain which unlike other plantar fasciitis worsens with activity(4). On palpation they'll be tender over the lateral or lateral aspect of the calcaneum and pain will be replicated by the squeeze test (see Figure 4). Plain X-ray or MRI could be used to validate the diagnosis.
Conclusion
This article has outlined several pathologies that needs to be considered when assessing clients with heel pain. Treatment modalities should be aimed at preventing pain and fixing potential predisposing factors.References
1. Aksahin E et al (2012) The comparison of the effect of corticosteroids and platelet rich plasma (PRP) for the treatment of plantar fasciitis. Archives of Orthopaedic Trauma and Surgery. Vol 132 781-785.
2. Alsahmi A, Souvlis T, Coppieters M (2008) A review of plantar heel pain of neural origin: Differential diagnosis and management. Manual therapy vol 13 103-111.
3. Anderson J, Stanek J (2013) Effect of foot orthoses as treatment for plantar fasciitis or heel pain. Journal of Sport Rehabilitation Vol 22 130-136.
4. BruknerP and Khan K (2012) Clinical Sports Medicine 4th edition McGraw Hill.
5. Chang R, Kent Bruan J, Hamill J (2012) Use of MRI for volume estimation of tibialis posterior and plantar intrinsic foot muscles in healthy and chronic plantar fasciitis limbs. Clinical Biomechanics. Vol 27 500-505.
6. Chen C, Lew H Chu N (2012) Ultrasound guided diagnosis and treatment of plantar fasciitis. American Journal of Physical and medical Rehabilitation, Vol 91 (2) 182-184.
7. Diaz-Llopis I et al (2011) Randomised controlled study of the efficacy of the injection of botulinum toxin type A versus
corticosteroids in chronic plantar fasciitis: results at one and six months. Clinical Rehabilitation Vol 26 (7) 594-606.
8. Diaz-Llopis et al (2013) Botulinum toxin type A in chronic plantar fasciitis:clinical effects one year after the injection. Clinicla Rehabilitation Vol 27 (8) 681-685.
9. Dizon J et al (2013) Effectiveness of extracorporeal shock wave therapy in chronic plantar fasciitis: A meta-analysis. American Journal of Physical Medicine and Rehabilitation Vol 92 no7 606-620.
10. Thomas J et al (2010) the diagnosis and treatment of heel pain: A clinical practice guideline-revision 2010. The Journal of Foot and Ankle Surgery. Vol 49 S1-S19.
11. Wearing S et al (2010) Plantar enthesopathy: thickening of the enthesis is correlated with energy dissipation of the plantar fat pad during walking. The American Journal of Sports Medicine Vol 38 (12) 2522-2527.
12. Winson L, Wong W, Kung E, Leung A (2012) Effectiveness of adjustable dorsiflexion night splint in combination with accommodative foot orthosis on plantar fasciitis Vol 49 (10) 1557-1564.