Injury scientist, Dr. Alexander Jimenez looks at a often misunderstood problem -- the 'high ankle' sprain...
Ankle injuries are prevalent in sport and the type of injury will fluctuate based upon the tissue structure injured in the complex. Ankle and the foot can be subject to impact loads in the performance of sport related activities the ankle can absorb six times body weight from activities. Because of this energy dissipation throughout the ankle, these forces may result in fracture and ligament disruption.
Lateral ligament sprains are undoubtedly the most frequent (85%) type of ankle sprain, accompanied by medial 'deltoid' ligament sprains and more infrequent is injury to the distal tibiofibular syndesmosis. It is thought that syndesmosis injuries comprise 1-20% of ankle injuries (Zalavras and Thordarson 2007; Hopkinson et al 1990); however this is very likely to be considerably greater in collision sports like football and rugby. Where a player was tackled by another, tibiofibular syndesmosis injuries often occur in contact situations.
The equilibrium of the distal tibiofibular syndesmosis is offered by the structure of the portion of the intervening ligaments and fibula and the tibia. Injuries to the syndesmosis, otherwise known as "high ankle sprains", many commonly occur when the foot is hyperdorsiflexed or rotated, or both (orthe foot is forced upward or outward) and are more common in sports like football, rugby, skiing, basketball, softball and wrestling.
Sports medicine professionals love that syndesmosis injuries or "high ankle sprains" are complex and difficult to diagnose and properly handle often with misdiagnosis and poor direction. Rehabilitate and therapists cite the syndesmosis as being one of the injuries that are most difficult to totally comprehend.
The outcome following a syndesmosis injury is the athlete attempts to return to competition only when they can't perform in the level due to pain from the ankle and/or malfunction in running and stepping action to be disappointed.
Therefore, diagnosis and early recognition is critical for a good outcome and to avoiding chronic problems. If needed surgical intervention is recommended.
Both part Rehabilitation Masterclass' objective is to describe in detail the things important in tibiofibular syndesmosis injuries, to highlight the assessment considerations and also to detail the rehabilitation program required after this rather difficult to handle sports injury.
Anatomy & Biomechanics Of The Syndesmosis
The ankle proper is called the joint and it is made up of the articulation between the talus bone in the ankle as well as the lateral malleolus of the tibia and lateral malleolus of the fibula. This joint is where authentic dorsiflexion and plantarflexion occur. The dome-shaped arrangement of the talus fits into the concave tibial undersurface and this arrangement is known as the ankle 'mortise'.Beneath the talocrural joint is the subtalar joint, formed by the talus. It's a gliding joint (like the hinge joint that's the talocrural joint) and this is the place where the ankle increases inversion and eversion, moves necessary for midfoot pronation and supination.
The joint amongst this complicated is the distal tibiofibular syndesmosis. The syndesmosis is a tough fibrous joint that allows fibula and the tibia to allow functional movement to happen in locomotion and to work collectively providing a congruent and stable joint for function.
The distal fibula articulates with the tibia through the vertically orientated fibula top notch (incisuria fibularis tibiae) found on the lateral tibia between the anterior and posterior tibial tubercles. They form the distal tibiofibular syndesmosis.
It has been shown (Lundberg 1989) which with active dorsiflexion of the ankle the talus glides posteriorly in relation to the tibiofibular joint. During movement and locomotion, against the mortise the talus will 'push' since the ankle approaches dorsiflexion and exert an outward force. This is a result of the distinctive anatomical arrangement of the talus with the anterior area of the talus being 4.2mm narrower than the anterior part. This causes a widening of the mortise as the anterior ankle wedges to the mortise with dorsiflexion (Norkus 2001). The talus in dorsiflexion exerts a force so degrees rotates, moves posteriorly and proximally 2-4mm 1-3mm as well as roughly 1mm is widened by by the mortise. These movements are reversed with plantarflexion.
Clearly the distal tibiofibular articulation needs to be a secure relation- ship to maintain the solid ankle 'mortise' but has to be flexible to allow the motion during stance and dorsiflexion.
To prevent the syndesmosis from widening during this motion, the following soft tissue structures encourage the integrity of the joint (Ogilvie-Harris et al 1994; Xenos et al 1995):
- Anterior inferior tibiofibular ligament (AITFL) -- supplies about 35% of power of the syndesmosis. This ligament is the most vulnerable to injury; syndesmosis ligament or poor tansverse ligament (ITL) -- 33%;
- Posterior inferior tibiofibular ligament (PITFL) -- 9%;
- Syndesmosis or interosseous ligament/ tissue (IOL) -- 22%.
If the ligaments are compromised, fibula and the tibia are allowed to proceed apart or 'gap' and also a diastasis develops. In this case the joint becomes secure.
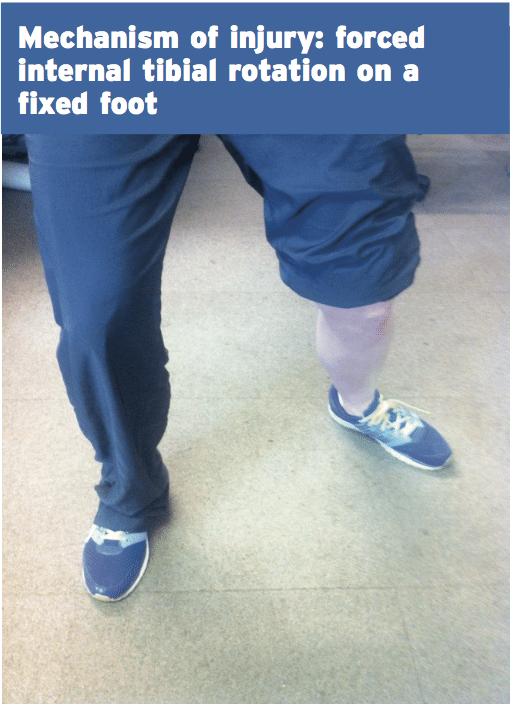
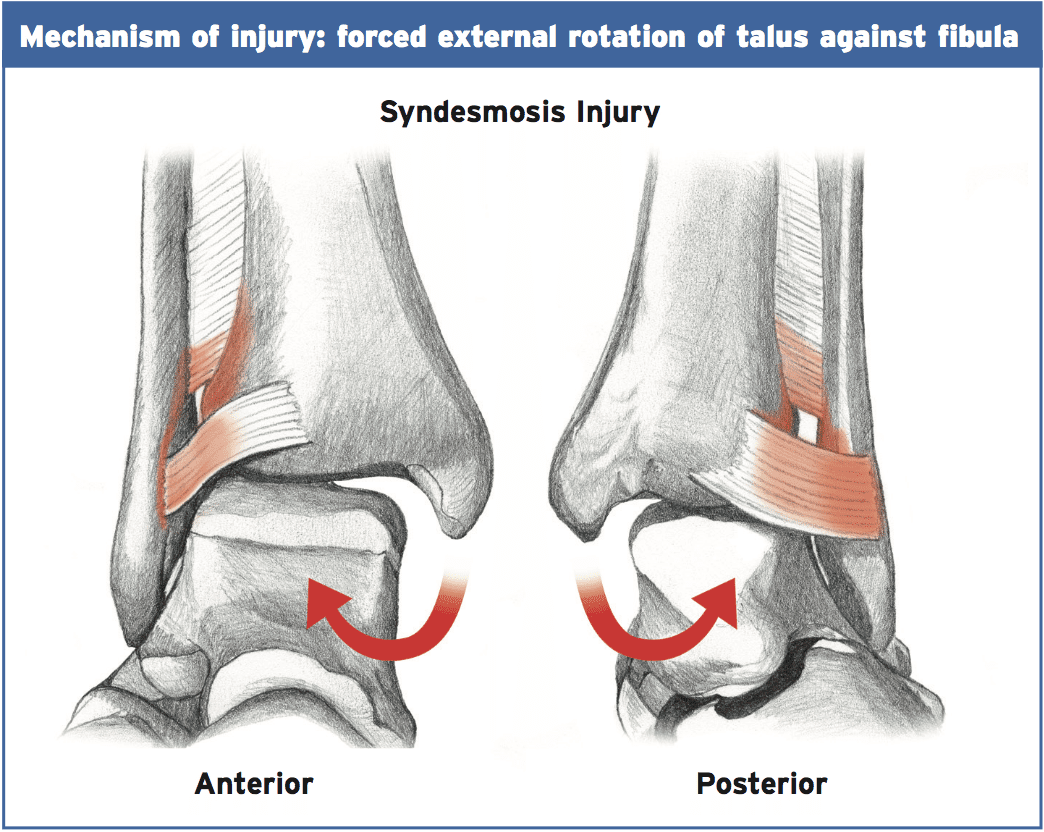
Mechanism Of Injury
Any step that widens the ankle mortise can damage the syndesmosis. In how much the injury progresses, the severity of the force and the length of the force are determining factors. The typical and normal mechanism of injury is forced closed kinetic chain external rotation of the foot with abduction and dorsiflexion of the ankle with forced internal rotation of the tibia. This classic mechanism could take place if the leg was caught under the body suddenly and the leg twisted on top of the ankle (because of fall or tackle), or when an athlete quickly changes direction whilst the foot has been fixed on the ground (usually the studs or cleats avoid any shear motion of the shoe-foot interface). A frequent example in skiing is really for the ski to stay in the snow and the ski imparts a solid and sudden external rotation on the foot.This rotation position of the foot/ankle moves the talus laterally and into rotation and the ankle mortise widens by abutting the fibula and forcing it laterally and posteriorly. Calcaneus eversion further widens the mortise and the lateral fibular is pushed from its articulation with the tibia. The ligaments are sequentially torn in order to posterior from anterior; hence the AITFL is almost always involved in all grades of injury.
The size and duration of the force at the time of injury determine the level of harm. Significant force and duration of force will damage PITFL, ITL, IOL and the AITFL. What's more, additionally damaged with this particular mechanism and it is not unusual for the external rotation force to be transmitted upward towards the superior tibiofibular joint. In this instance, the athlete may whine of co-existing lateral knee pain (Seymortier et al 2008).
Types Of Injuries
Grade 1 (sprain without diastasis)A typical low velocity and/or very low force external rotation-type mechanism that's strong enough to 'gap' that the mortise will make an injury to the thoracic ligament as the talus rotates laterally and the distal syndesmosis may marginally separate, hammering the AITFL. This force is generally inadequate to injure the deeper behind structures like the interosseous membrane or the deep deltoid ligament on the medial side.
The AITFL will probably be tender to palpate. AITFL injury's degree may vary from a strain to some significant strain/tear; nonetheless, since the syndesmosis remains intact the injury is considered to be stable.
Therefore grade 1 injuries by definition are stable, but the level of AITFL damage may be classed as grade 1 (minor but steady injury) to more acute AITFL damage (important but stable harm).
Grade 1 injuries can be successfully managed conservatively within an Aircast walking boot for a time period (mentioned later).
Grade 2 (diastasis clear on stress radiographs)
This involves a greater level of dorsiflexion/external rotation force and also entails damage to:
- anterior deltoid ligament (complete disruption usually);
- deep deltoid ligament;
- significant tear in AITFL;
- interosseous ligament.
These type of injuries are often tricky in that the instability may be overlooked originally and treated as a secure syndesmosis with early mobilization and early return to running. Typically, if these are misdiagnosed and thus mismanaged, a poor outcome will result leading to operation at a later stage. A mismanaged syndesmosis may then lead to a chronic and shaky ankle which may predispose the athlete to ongoing pain, further injury, arthritic changes and osteochondral lesions.
Some exact low-level tier 2 injuries can be managed conservatively surgical intervention will be needed by the injuries. This is the type of injury that most commonly gets mismanaged as frequently they are suspected of being adequate for conservative management as the mortise heals in a widened position with talus motion in the mortise, they do to function.
Grade 3 injuries (frank diastasis)
This involves abduction of the foot and external rotation. This will result in severe injury to the syndesmosis (AIFTL, PITFL, interosseous ligament and membrane) as well as complete disturbance of the deltoid ligament. This is often associated with fracture of the distal fibula (Masionneuve fracture). When there is, syndesmosis rupture is supported on x-ray.
Widening of the medial clear space in connection with extending of the tibiofibular interval in the level of the ankle, and these are observed on non-weight bearing x-ray that is regular. These injuries are unstable on standard radiographs and management will demand a surgical intervention.
Examination
Subjective
The athlete will often complain of pain that is intense at the distal tibiofibular joint which makes it tricky to weight bear. They may also complain of knee pain if the proximal tibiofibular joint is involved. The incident may be remembered by them as mimicking the mechanism of injury like the foot being captured under the body and they twisted on top of the foot.Knowing the exact mechanism of injury is vital in identifying a lateral ankle sprain when compared with a high- tier syndesmosis injury. The prior can be handled whereas the latter will want a stabilization operation for your syndesmosis.
What's more, willingness or the ability to weight bear also can be a indicator that is decent. Often lateral ankle sprains have the ability to weight bear early whereas injuries with or without fracture will be reluctant to burden bear.
A missed shaky syndesmosis injury that is not properly treated can result in outcome and prolonged morbidity. Hence getting the diagnosis is vital.
Objective
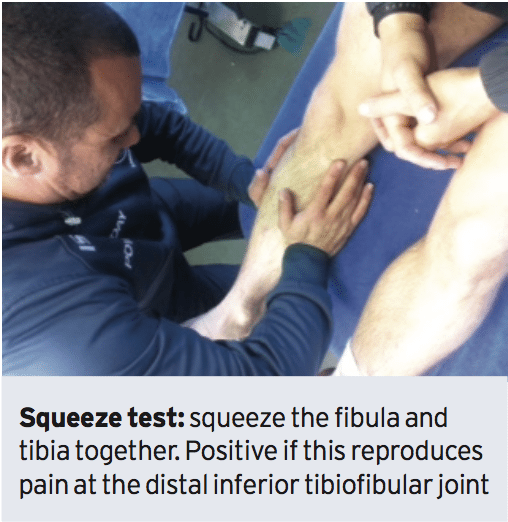
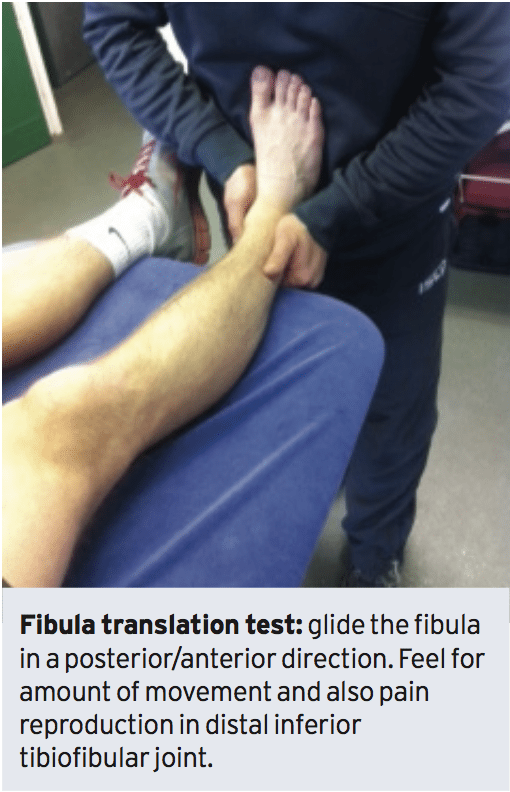
No single goal test is legitimate for confirming a syndesmosis injury (Sman 2013).Confirmation is usually made on the answer as well as history on numerous evaluations. It has to be mentioned that in severe syndesmosis sprains many if not all of these tests may be due to pain, spasm and swelling. Often the initial suspicion is based on mechanism of injury and also palpation pain.
1. Gait. Typically if the individual is able to partially weight bear they will do so about the forefoot (walk on toes) as this normally avoids dorsiflexion that probably will be painful.
2. Palpation. The deltoid ligament will be tender to palpate along with the AITFL are also tender. At a high-grade syndesmosis that the palpation pain will expand a way up the fibula. Often the lateral ankle ligaments (ATFL, CFL) will not be tender, especially in dorsiflexion/external rotation mechanisms.
3. Swelling. Swelling over the joint line between the tibia and fibula is often indicative of syndesmosis injury.
4. Squeeze test. A non-weight posture evaluation where the mid shaft of the fibula and tibia are squeezed and pain is felt at the distal syndesmosis. The compression of the bones will create an opening effect on the distal tibiofibular joint. It has been shown to be a good prognostic indication for length of absence.
Investigations
1. X-ray. Routine x-rays (AP, lateral and mortise views) will probably be needed to exclude fractures of the fibula, avulsion injuries and talar dome fractures. To see syndesmosis injuries that are unstable stress x-rays will be necessary to gauge the amount of separation. Due to the pain this repeats, a local anaesthetic block might be required to fully stress the joint. Externally rotating the foot or simply by having the athlete stand on one foot applies stress. On x-ray the medial clear space (should be less than 4mm) and lateral clear distance (should be less than 6mm) can be quantified and also the tibia-fibula overlap which should be greater than 1mm on all views. Stress views will reveal anterior and lateral displacement of the fibula compared to viewpoints.2. CT. These are somewhat more sensitive than x-rays in discovering a injury and these can detect differences as small as 1mm.
3. MRI will show the anatomical injury. It is used to identify AITFL, interosseous and PITFL injuries, osteochondral lesions and bone bruising.
4. Arthroscopy. This can be used to validate a suspected syndesmosis injury found on imaging. With arthroscopy, the ligaments may be assessed and an arthroscopic stress test could be conducted to evaluate instability. Furthermore talar dome lesions could be assessed under arthroscope.
A positive diagnosis to get a injury usually involves a mix of factors:
1. A typical history with a expected and typical mechanism of injury;
2. The location of pain focused the tibiofibular joint round with degrees of pain along the fibula and possible ligament pain;
3. An inability to weight bear;
4. Favorable signs on a number of the evaluations;
5. Imaging which could show uncertainty on anxiety viewpoints on instability or perspectives;
6. If accessible, MRI and CT can confirm the degree of tissue damage and joint separation.
The potential differential diagnosis that may mimic a syndesmosis injury include:
1. Lateral ankle sprain;
2. Fibula fracture in the absence of syndesmosis soft tissue injury;
3. Osteochondral lesions on the talar dome;
4. Capsular sprains of the anterior ankle;
5. Retinculum strains without underlying tibiofibular joint damage.
Summary
Injuries are ankle injuries seen from the population. The normal mechanism is a forced external rotation of the foot/ankle in regard to the tibia and fibula. It is more common in contact sports and skiing. The athlete can present with a ankle with pain/ swelling present on the inferior tibiofibular joint and potentially along the fibula and involving the superior tibiofibular joint. Timeless syndesmosis clinical evaluations may prove inconclusive because of the lack of specificity and sensitivity with some of these tests. Imaging such as anxiety perspective x ray and more sensitive MRI may be required to confirm the diagnosis.References
1.Athletic Therapy Journal. Sept 2002.
2.J Bone and J Surgery Am. 1976. 58(3); 356-357.
3. Foot Ankle Clinic. 2009. 14(2); 277-298.
4. Foot Ankle. 1990. 10(6); 325-330.
5.BJSM.2013. 0; 1-7.
6.American Journal of Sports Med. 2012. 40(10); 2348-2356.
7.J Athletic Training. 2012. 47(3); 339-357.