Chiropractor, Dr. Alexander Jimenez looks at injuries in the Lisfranc joint — and how they may be treated.
Foot injuries are common in the athlete and they appear in many forms. These include sprains into the joints between the tarsals and metatarsals , chronic soft tissue injuries such as plantar fasciitis and stress fractures of the metatarsals and tarsal bones. Injuries to the midfoot and in particular the Lisfranc joint (or tarsometarsal joint) are a rare but potentially devastating injury to the sportsperson that require particular attention by the sports medicine practitioner.
Athletes were not involved by the type of the injury but involved personnel. Surgeon Jacques Lisfranc Saint Martin first described it who performed midfoot amputations on soldiers through the ‘Lisfranc’ joint after they’d dropped off their horses.
In present day scenarios, accidents to the joint are often high velocity injuries that cause severe deformity into the midfoot joints due to dislocations. These energy mechanics would be the result of a car/motor bike Collision, severe fall on the foot or a severe injury to the foot usually lasted in an industrial setting. From the athlete, injury severity is usually far less devastating and results from some form of crushing and/or twisting mechanism. But if it occurs it can have devastating consequences for the athlete.
Introduction
Although foot injuries in the athlete are reasonably common (16 percent of sports-related accidents involve the foot — Garrick and Requa 1988), accidents to the Lisfranc joint are extremely rare. Myers et al (1994) discovered that Lisfranc injuries account for 4 percent of collegiate-level football injuries. However, the forms of the harm can’t just be career-ending although season-ending for the athlete.It is more typical in sports like American Football (using a high percentage of Lisfrancs happening in offensive linemen — Myers et al 1994) and rugby since these sports involve high levels of touch which may involve force throughout the foot and the harm has also has been seen in horse riding, windsurfing, baseball, rodeo riding, gymnastics and skydiving.
Relevant Anatomy
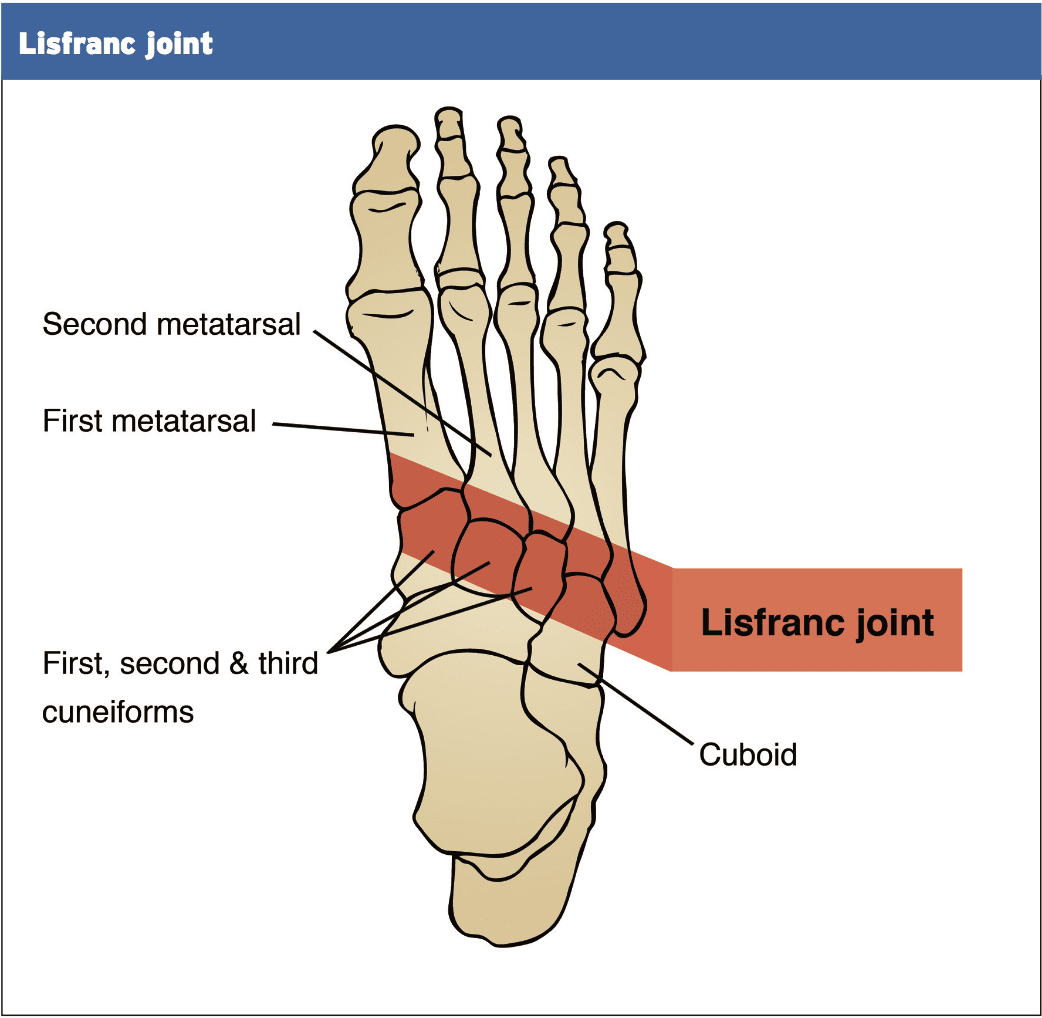
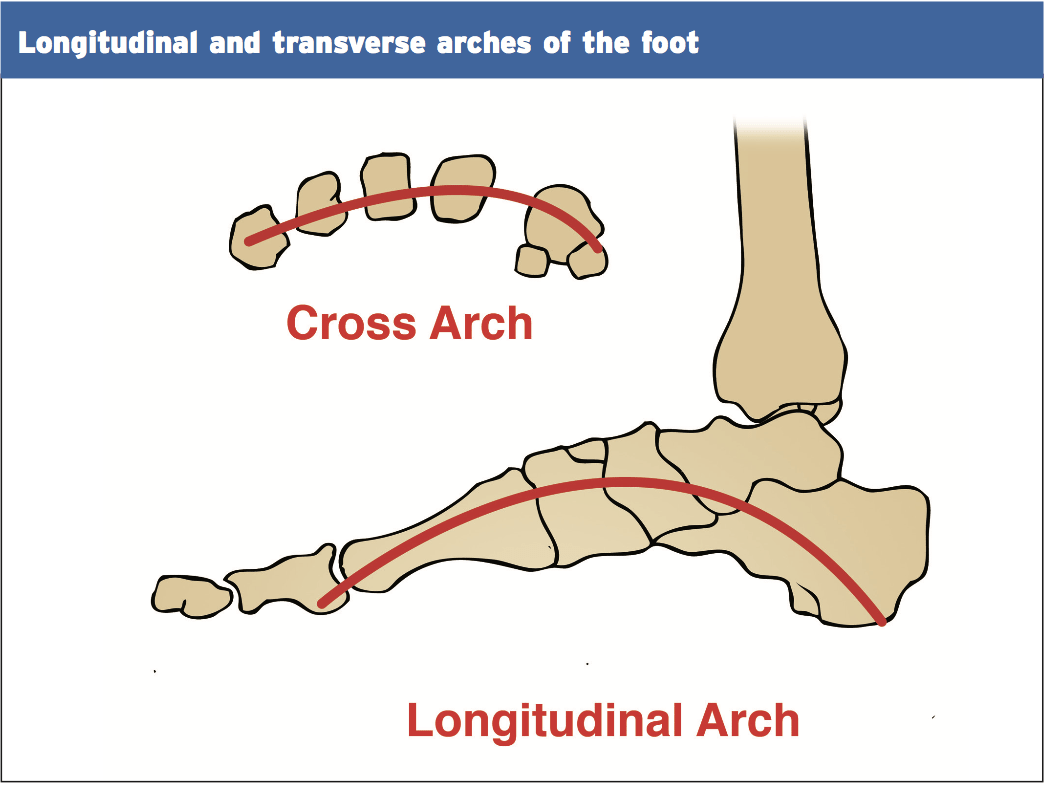
The support of the midfoot is derived from the dorsum of the foot, the supporting ligaments as well as the extrinsic and intrinsic muscles that span the plantar arch and the skeletal constructions. The Lisfranc complex is a broad term that defines the articulation between the midfoot and forefoot. It comprises the joints between the proximal row of cuneiforms and cuboid with the distal row of metatarsal heads and harm to this ‘zone’ of articulations may come in many variations.
The architecture’s concave structure makes for a structure like a ‘Roman arch’. Therefore along with the ligaments that are rigid, the architecture of the midfoot is stable and inherently very strong on the plantar aspect of the foot to avoid collapse of the arch.
The Lisfranc joint is comprised of three main segments (Chiodo and Myerson 2001 and Ouzounian and Sheriff 1989):
1. Medial column. The articulation between the medial cuneiform and the first metatarsal. This allows 3.5mm of dorsal plantar movement.
2. Middle column. Its articulation with the lateral and the middle and medial cuneiform and the recessed second metatarsal cuneiform. It’s greater stability as this joint is recessed more proximally than another metatarsals. This creates the ‘keystone’ . The cuneiform and the metatarsal make up the center column. This has less than 1mm of motion.
3. Lateral column. The articulation between the cuboid and the fifth and fourth metatarsals. This is definitely the most mobile with up to 13mm of motion.
The three columns are separated by three distinct synovial capsules and so constitute three non-communicating synovial systems (Castro et al 2010).
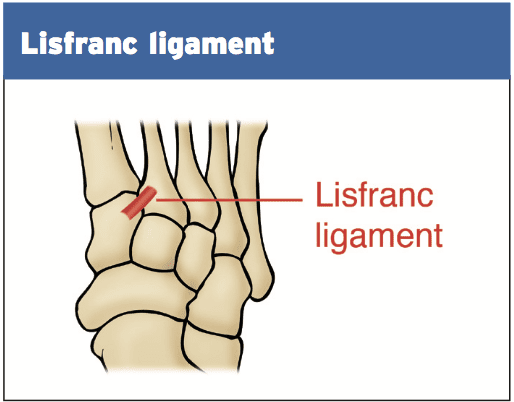
The interosseous ligaments stabilize these bones. However, the base of the metatarsals don’t have any interosseous ligament. The second metatarsal is joined into the cuneiform via the cutaneous ligament called the ‘Lisfranc’ ligament.
Classic Mechanism Of Injury
Additional tendon insertions support the midfoot. The tendon insertions of the tibialis anterior (to the dorsum of the first metatarsal base and lateral cuneiform), the peroneus longus (attaching into the lateral and lateral aspect of the first metatarsal) and the tibialis posterior (attaching into the navicular so this indirectly controls the position of the arch). At length, the plantar fascia as well as the intrinsic foot muscles may add the plantar arch and further support.Mechanisms Of Injury
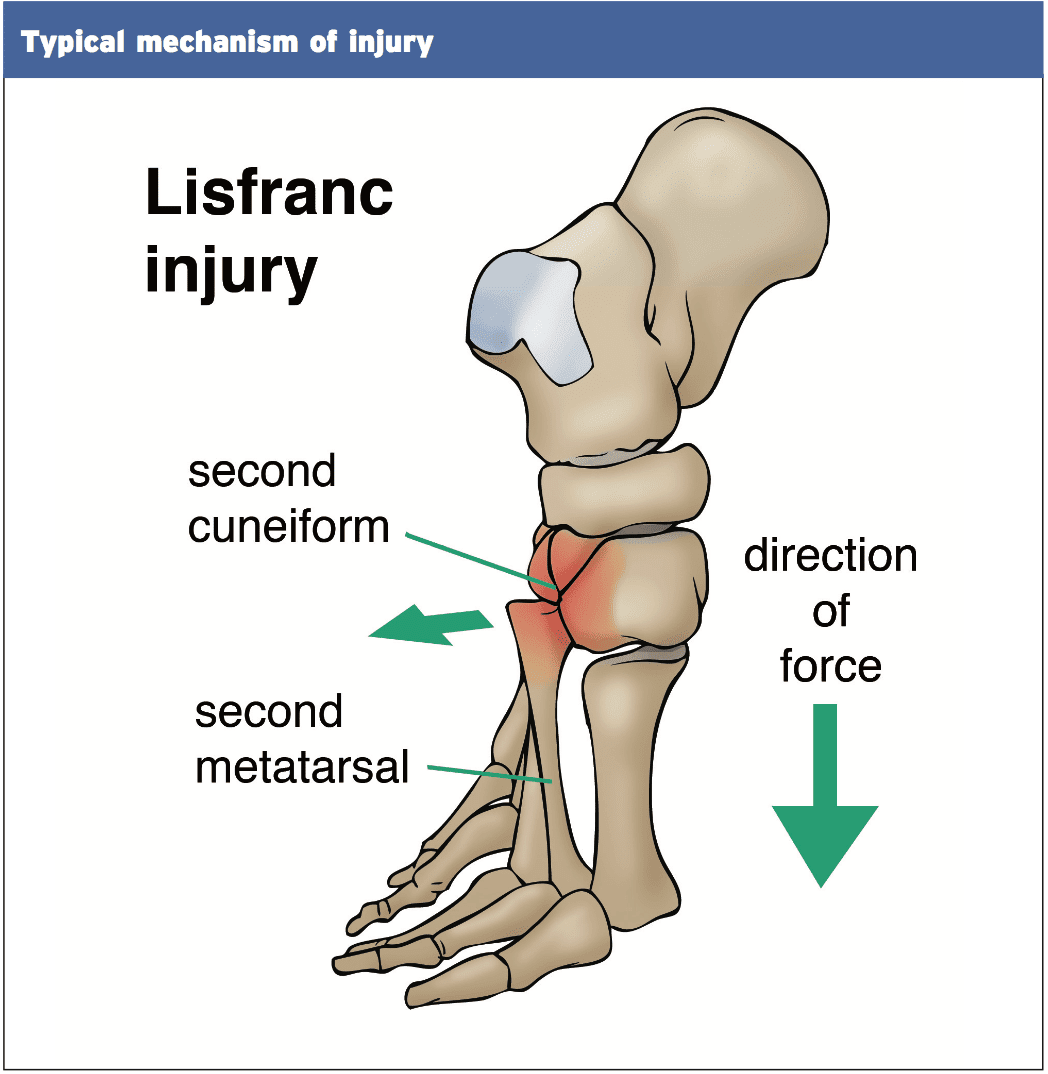
The mechanism of injury to the midfoot can be categorized as low energy or high energy. The high energy variations involve motor vehicle accidents and almost demand some form of fracture and midfoot dislocation and will not be considered.1. Hyperplantarflexion of this midfoot if the foot is fixed. Horse riders and windsurfers commonly affect as the foot is fixed by means of a strap. The foot remains bound as the surfer/rider drops backward and the foot is forced by the weight of their body . Here is the mechanism that has been described by Dr Lisfranc years ago when he detected cavalry men fall from the horses.
2. Blow to the heels whilst foot is locked in plantar flexion. This occurs when the foot is shoving off and a weight drops onto the rear of the heel and compels a compression down the heel to the midfoot. This happens in football where a participant is going to push off and then a player falls on this foot whilst the foot is in a plantar flexed position, or it may occur in skydivers who land with the foot caught under these in plantar flexion (Shapiro et al 1994).
3. A injury to the foot since the foot is in a place that is weightbearing and pronated. This is not as common because of the unique anatomy of the midfoot joints whereas the plantar ligaments are a lot stronger than the dorsal ligaments (see anatomy and biomechanics); but a strong compression force throughout the midfoot may stretch and damage the plantar ligaments of the Lisfranc joint.
Due to the strength of because of the forces struck on the foot in injury mechanics, and the plantar ligaments in comparison using the ligaments, dislocations in a direction are considerably more prevalent than dislocations.
Signs & Symptoms
Many injuries to the Lisfranc can be difficult to detect and be subtle as many of the low energy accidents may go undiagnosed. Other distracting injuries like foot fractures or foot injuries might cause the examiner causing the more subtle Lisfranc injury.Often the athlete will find it tough to describe the original mechanism of injury when the injury additionally involves damage. Since these are deeply debilitating, the athlete might remember the foot was ‘twisted’ and ‘crushed’ although maybe not recall the direction or mechanism that the foot has been in.
Upon presentation (that can be days or weeks following the injury), the foot will be debilitating at the midfoot on the dorsal aspect over the Lisfranc joint and generally in the plantar arch as the intrinsic foot muscles will reveal palpable spasm as a protective mechanism.
The key characteristics in evaluation is:
1. In walking, especially push-off.
2. Palpation pain over the aspect over the first joint and then using the tarsals involving the metatarsals and their following articulations.
3. Swelling within the midfoot which may be diffuse and conceal the veins which may be observable on the unaffected side.
4. Eccymosis/bruising in the arch.
Special tests:
1. Pain of the dorsiflexion on the very first tarso-metatarsal joint with forced/ abduction of the forefoot.
2. Anxiety about squeezing the metatarsal heads.
3. Piano key evaluation — grasping each toe individually and moving them in a direction that is dorsal and plantar.
Imaging
X-raysThree viewpoints minimum ought to be under- taken, rather in both non-weight- weight bearing and bearing positions. These views include:
1. AP;
2. 30° oblique;
3. Lateral.
The tell tale signs to look out for include:
1. Fracture at neck or the base of the metatarsals.
2. Little avulsion in the base of the second or first metatarsal. A ‘fleck’ signal is described because of avulsion of the Lisfranc ligament as a small avulsion fracture of the base of the second metatarsal.
3. Orientation of the metatarsals to their corresponding tarsal bones (seen on AP viewpoints for first/second metatarsal and 30° oblique for fourth/fifth).
4. Displacement between the second and first metatarsal heads. Any greater than 2mm is diagnostic for a Lisfranc injury (seen on AP view).
5. The medial cortex of the fourth metatarsal must line up with the medial border of the lateral cuneiform (seen on 30° oblique view).
6. No disturbance of the dorsal cortical lineup of the first metatarsal into the medial cuneiform (viewed on lateral non-weightbearing perspective)
In a recent analysis by Rankine et al (2012) it was discovered that strategy AP radiographs and 45° views missed just over 30 percent of subtle Lisfranc joint separations. The suggestion was that the 30° view was sensitive to extending of the second and initial meta- space and that CT imaging was preferred for assessing joint diastasis.
CT Scan/MRI
CT scans can also be useful in assessing the widening of the joint spaces in addition to detecting any associated fractures. The CT will help the identification of a diastasis and may be utilized in conjunction with the x-ray formulate and to plan surgery.Although not routinely used, MRI can be used to evaluate any soft tissue injuries in connection to the Lisfrancs such as important tendon disruption (such as the peroneus longus tendon).
Classification
Nearly all classification systems utilized for Lisfranc injuries relate to the severe high energy kind trauma injuries (Myerson et al 1986). For the purposes of this guide, the classification by Nunley and Vertullo (2002) will be utilized as it’s more appropriate for the athletic population’s Lisfranc injuries. They talked about three aspects that led to the Level of harm1. Skill to weightbear;
2. Nearby point tenderness over Lisfranc ligament;
3. Radiographic appearance of the joint.
The three phases of Lisfranc injury are as follows:
Stage 1
- Able to weightbear cannot return to play.
- Locally tender over medial aspect of TMT joint.
- Radiologically reveal no greater than 2mm between initial and second MT without a collapse of the arch as quantified by the metatarsal vertical distance.
- Willing to partly weightbear; nonetheless, cannot return to play.
- Very tender on medial element of TMT joint.
- As measured by the cuneiform-fifth metatarsal vertical distance radiologically revealed diastasis involving 2-5mm between first and second MT without a collapse of the arch.
- Inability to weightbear
- Really tender aspect of TMT joint over.
- Diastasis greater than 5mm, collapse of arch.