Chiropractor, Dr. Alexander Jimenez looks at the hamate, the most frequent mechanisms of injury, common clinical features that would make a clinician suspicious of a hook of hamate fracture — also summarizes some treatment choices.
Introduction
Hook of hamate fractures are described as a often overlooked and rare injury . They are reported to account for only 2% of all carpal fractures and occur most commonly in athletes when the hook of the hamate abuts from a handle of a bat/club whilst swinging (2). Since by imaging the symptoms can be vague and may be overlooked, a delay in diagnosis is common. This delay in diagnosis increases the risk of union of the hook and rupture of the flexor tendons, therefore excision of the hook is advised.Anatomy
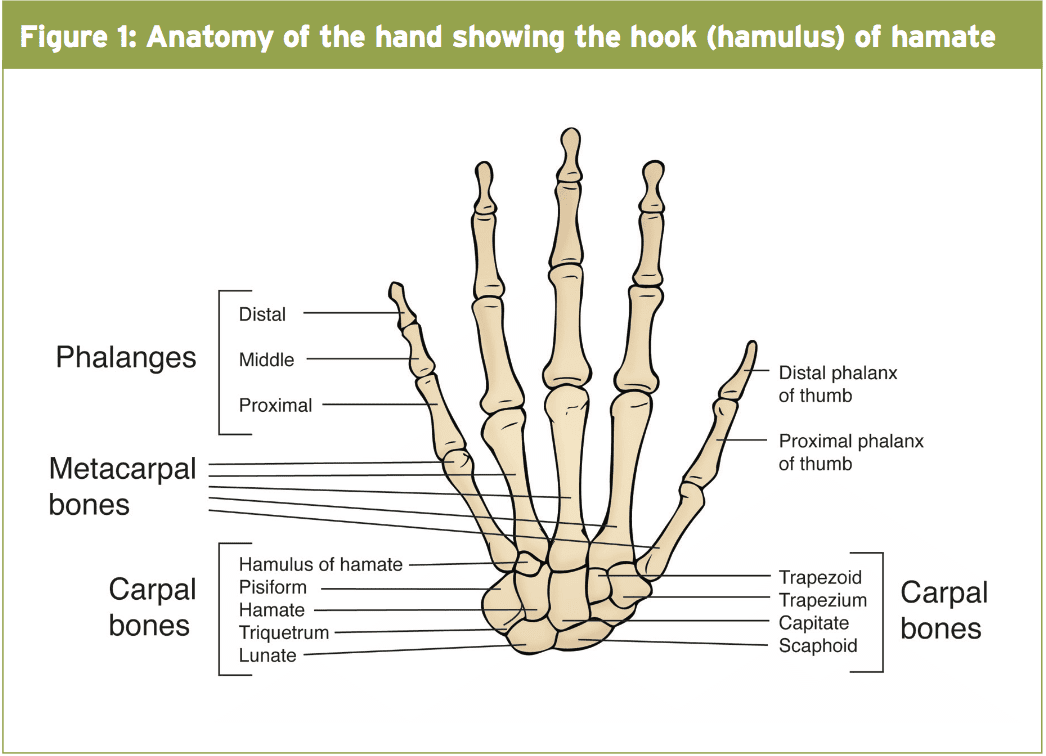
The hamate bone sits on the ulna side of the row of the carpal bones and also articulates with the fourth and fifth metacarpals distally, radially using the capitate and proximally with the lunate and triquetrum(6). It has an osseus prominence which protrudes volarly which will be the hook or hamulus(3) — (see Figure 1). The hook of hamate is an attachment site for both the transverse carpal and pisohamate ligaments as well the origin for the flexor digiti minimi brevis and the abductor digiti minimi muscles(3). These attachments give stability but they exert forces that are distracting to it. These distracting forces are considered one of the reasons why hook of hamate fractures have a higher speed of jelqing(6). As well as being an attachment site it also serves as a pulley for the flexor digitorum profundus tendon with gripping within an ulna-deviated place(3).Mechanism Of Injury
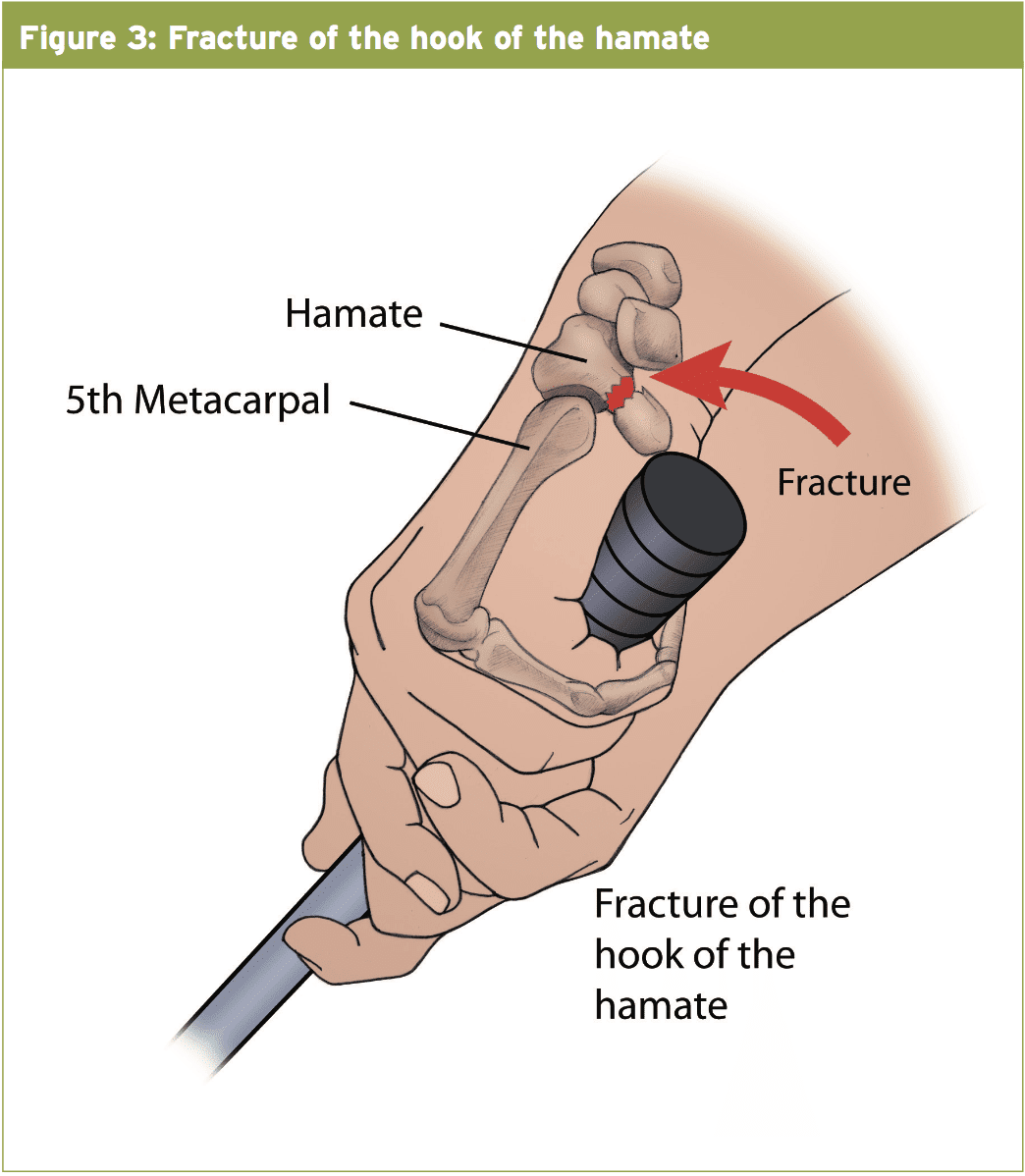
Fractures of the hook of hamate could be described as occurring by either indirect or direct forces. Most commonly by forces when the handle of a bat or bar abuts from the hook in a shot. Baseball players and golfers tend to fracture their non-dominant hand as this is where the hook makes contact with the bat/club — (see Figure 3). In golfers, fractures tend to happen when the club strikes the ground but in baseball these fractures tend to occur at the end of a forceful assessed swing as opposed to swings which make contact with the ball(two). Occasionally these fractures are seen in racquet sport athletes (tennis and racquetball) to the side once the athlete loses control of the racquet whilst attempting to make a shot(2). Occasionally fractures of the hook have been seen after a fall onto a dorsiflexed wrist(1).Clinical Presentation
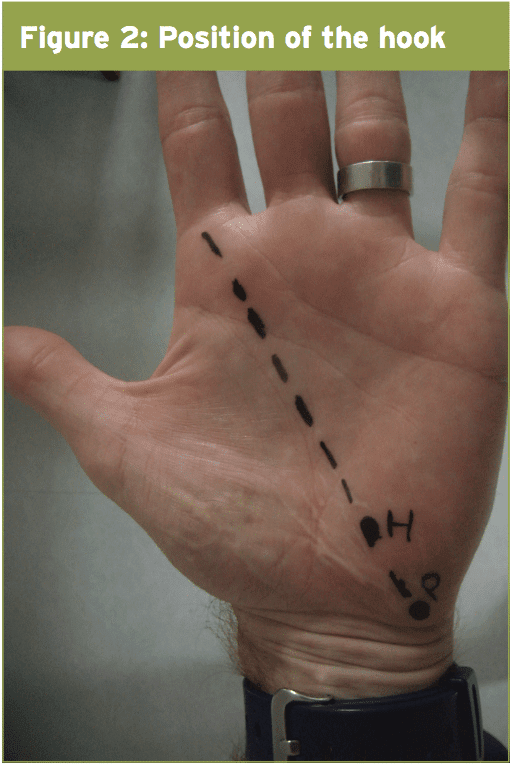
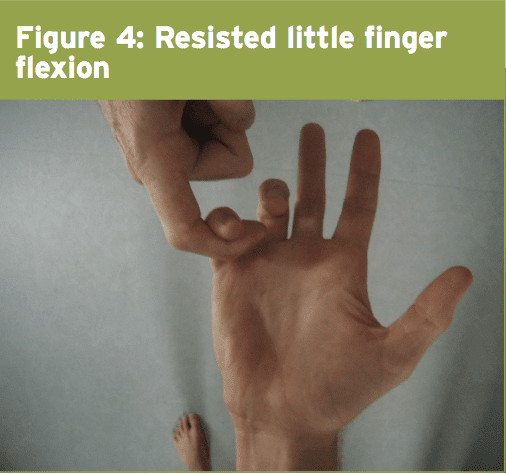
Athletes will often describe a vague ulna- sided wrist or hand pain(3). On most events patients can remember the specific moment of harm nonetheless, many studies have clarified hook of hamate fractures in which the athlete doesn’t recall a particular incident or drop(1,5). No matter the mechanism, all patients reported point tenderness over the hook(2). Interestingly, tenderness can be often noted on the dorsal aspect of the hamate as well(two). The website of maximal tenderness might be misleading since the thinly-covered dorsolateral aspect of the wrist could be more painful especially if the fracture is in the base of the hook(5). Due to the proximity of the branch of the ulnar nerve into the hook, some patients might also have paraesthesia in the ulnar nerve distribution. Pain on passive or active wrist extension and pain with grasping tasks particularly in ulna deviation can also be reported(5). As described previously, the hook acts as a pulley for the flexor digitorum profundus tendon and as these a small finger flexion may even commonly elicit pain — (see Figure 4).Imaging
When a hook of hamate fracture is suspected imaging is required. Regular postero-anterior and lateral views of the wrist normally forget a hook of hamate fracture(3). A carpal tunnel view is described to obtain to get a hook of hamate fracture. But this radiograph can be tough to obtain as it requires forced wrist extension that might be painful in the acute setting(3). CT scan has been shown to have a greater sensitivity (100%) and specificity (94%) compared to traditional radiographs whose sensitivity is 72 percent and specificity 88 percent. CT scan has the advantage of performing bilateral comparison and may identify other congenital variants(2). MRI has been shown to be a good option in this setting.MRI has the advantage that it shows other soft tissue structures around the area including the neurovascular bundle and triangular fibrocartilage complex also identifying other potential causes of pain, ie ganglia(3).
So differentiation between also a fracture and a non-united ossification facility should be considered, ossification isn’t complete until the age of 15. A non-united ossification center will on CT have margins that are corticated whereas a fracture will have edges that are irregular and won’t be corticated. A current fracture may have bone oedema on MRI and bone scan will reveal increased uptake on a fracture although not a unfused ossification center(6).
Direction
Management’s two main classes are conservative management which involves a period of operation or immobilization which includes either open reduction internal fixation or excision of the hook.Acute fracture
If a patient presents with a hook of hamate fracture less than four months old and it’s minimally displaced (less than 2mm) then a period of immobilization should be trialled(3). Studies report a recovery rate of 17-46% after immobilization in a short arm cast from proximal forearm into the PIP joints of the ring and small fingers for six to eight months(3). The cast must prevent any regeneration of the flexor tendons since these pull the fracture website into the ring and small fingers diminishing the opportunity of union. Some authors assert as a result of the very low recovery rate that excision of the hook should be carried out in most cases as this operation was shown to have good to excellent benefits and a return to previous amount of activities in six to eight weeks(6 weeks).Intense displaced fractures can be treated by open reduction internal fixation (ORIF) or excision of the hook. Most writers agree that excision is the preferred option in this scenario(two).
Chronic Fracture
Delayed diagnosis is common as I have outlined and as a result non-union or partial marriage is frequently seen. It’s thought that poor marriage is not because of inadequate blood supply (such as from the scaphoid) but more due to ongoing forces being transmitted through the fracture site in soft tissue structures(two). Non-united fractures can be broken up into painless and painful. Painful non-united or partially united fractures should be treated with excision of this hook(2). This has a low complication rate (3%) and athletes have been shown to be able to go back to previous level of activity in six to eight months(2,6). Potential complications include fatigue, altered sensitivity and scar tenderness that generally all resolve in a few weeks(two). Reports of median and ulnar nerve injury also have been described(2). In this procedure the whole hook should be excised, as re-fracture has been seen in athletes in which just the tip of the hook was excised(6).Following resection of the hook to the bottom, wrist and the hand would be immobilized in a splint or cast for 2 to three weeks. From three weeks that the athlete could commence rehabilitation and ought to aim to return to full activity at six to eight weeks(6 weeks).
Controversy surrounds the therapy of marriage or a. Most writers recommend excision of this hook because this prevents Fig rupture which is a typical late complication regarded as attributed to FDP and FDS tendons rubbing the irregular surface of their non united hamate(2). Total rupture has been reported in 15-20% of cases. The tendon into the little finger ruptures first followed by the ring finger tendon. When it does occur then treatment of the tendon and excision of the hook is advocated. Others advocate waiting for tendon signs or signs to present before excision(2).
Conclusion
Hook of hamate fractures might not be as rare as previously thought and they need to be suspected in athletes with obscure ulna- sided hand or wrist pain. So CT or MRI should be utilized to validate the existence of a separation routine radiographs will frequently forget a fracture of the hook. Management may be healed with by A non-displaced intense fracture but the healing rate is low as a result of diversion forces of the tissues that attach onto the hook. Late or early surgical excision of the hook has excellent results with minimal danger. Excision of the hook also reduces the possibility of rupture of the flexor tendons which is not uncommon in non-united fractures. Reports show return to sport six to eight months post- operation. The clinician ought to be suspicious of a hook fracture as stress fractures of the hook also have been reported, when the athlete doesn’t report a specific event.References
1. Ardevol J, Henriquez A (2002) Hook of Hamate Non union: suspicion of stress induced mechanism in a hockey player, Vol 10 pg 61-63
2. Binzer T, Carter P (1996). Hook of Hamate Fracture in Athletes. Operative Techniques in Sports Medicine, Vol 4, No4 pg 242-247
3. Briones M, Aldridge M (2010). Hook of Hamate fractures. Operative techniques in Sports Medicine, Vol 18 134-138
4. David E et al (2003). Symptomatic, partial union of the hook of hamate fracture in athletes. The American Journal of Sports Medicine Vol 31, No1 106-111
5. Guha A, Marynissen H (2002). Stress Fracture of the hook of hamate. British Journal Sports Medicine. Vol 36 pg 224-225
6. Parker et al (1986) Hook of Hamate Fractures in Athletes. The American Journal of Sports Medicine. Vol 4, No 6 pg 517-523