Studies suggest that between 3 and 9 percent of all sports injuries involve the hand or wrist. Chiropractor, Dr. Alexander Jimenez examines ulnar impaction, among the more common injuries to affect this region, particularly among older athletes…
Ulnar impaction syndrome (UIS — sometimes called ulnocarpal abutment) is a condition where the ulna of the forearm is too long relative to this radius, resulting in excessive loading on the ulnar side of the wrist. Ulnar impaction syndrome could be secondary to shortening of the radius, although this condition is congenital and present from birth. Regardless of the origin, however, most patients become symptomatic in life, when accumulated and degenerative wear and tear takes its toll on both the ligaments and cartilage, resulting in wrist pain. For athletes whose sports involve loading of their limbs, this can be a problem.
Wrist Stability
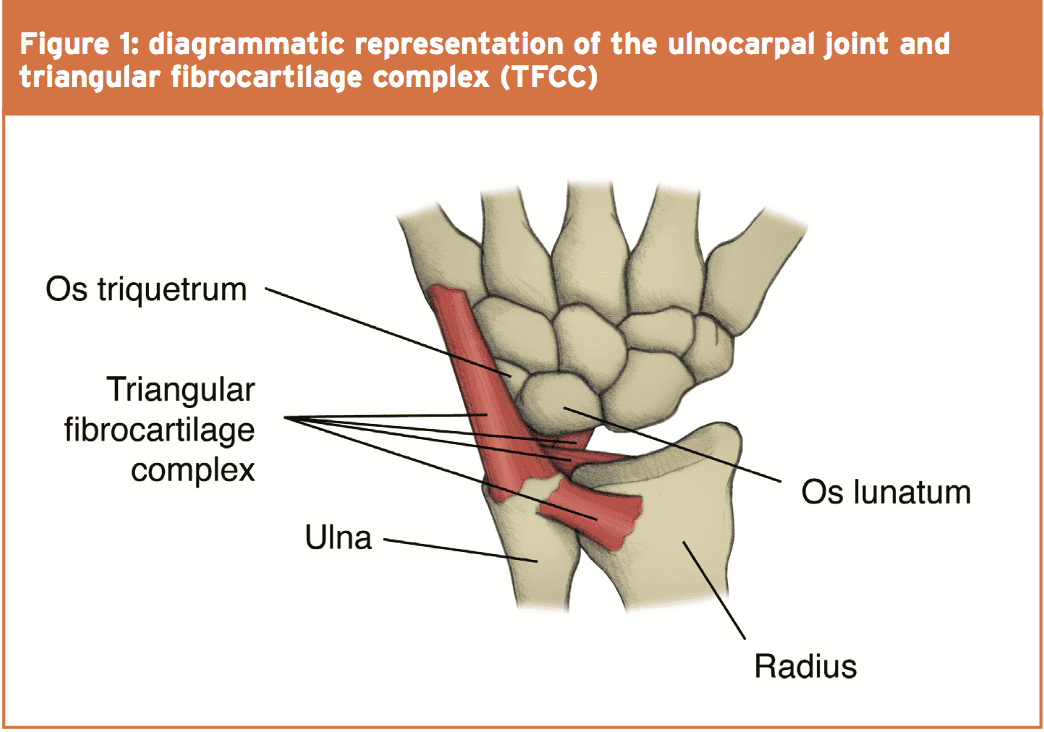
To appreciate ulnar impaction may result in ulnar-sided wrist pain, it will help to comprehend the structure and function of the triangular fibrocartilage complex (TFCC) and loading across the ulnocarpal joint (see Figure 1). Wrist stability is improved an arrangement of ligaments and fibrocartilage, via the TFCC arising from your sigmoid notch on ulnar border of the radius and inserting into the base of the ulnar styloid and fovea of the ulnar head.While it connected with congenital or acquired positive ulnar variance, UIS can also happen in ulnar neutral or even negative ulnar variance wrists(4,5). Athletes doing power and/or grasping activities connected with axial loading and rotation are especially at risk of ulnar impaction syndrome because of their ‘dynamic ulnar variance’ that occurs during tasks requiring maximum traction and pronation(6). More commonly events which set compression and rotation demands on the upper limbs increase the risk of ulnar impaction via traumatic development.
Although symptoms of UIS rarely present in athletes, the risk for all these symptoms in later life could be increased by events during those formative years. One reason for this is that distal radius fractures are the most frequently occurring fracture in children under the age of sixteen. Research shows that when significant radial shortening (5mm or more) happens as a result of these fractures, there’s a considerably increased probability of long-term operational impairment (7). Additionally, even in the absence of distal radius fractures, we know that submitting an immature wrist into prolonged compression and insistent micro-trauma has can result in a premature arrest of radial growth plate and following ulnar overgrowth(8,9), and that of course greatly raises the risk of UIS in later decades.
Symptoms Of Ulnar Impaction Syndrome
UIS’s development Results in the degeneration and abutment of TFCC or the ulna against the ulnar carpus. Although any athlete could suffer from this racquet, gymnasts, boxers, illness and adhere sport athletes are particularly at risk, together with symptoms of pain particularly occurring during wrist rotation. It is important to comprehend, however, the development of this problem is not always linear; the load-bearing demand put on the TFCC means that there is a heightened susceptibility towards an acute traumatic injury, in addition to the secondary degenerative concerns implicated with ulnar impaction(10).Common symptoms of ulnar impaction syndrome include the following:
- Pain (especially during spinning), aggravated with activity and (normally) relieved with rest;
- Painful bending or clicking during pronation and supination;
- Occasional edema;
- Reduced wrist Assortment of motion;
- Decreased forearm rotation;
- Tenderness to palpation dorsally, just distal to the ulnar head and just volar into the ulnar styloid process;
- Each of the above tend to be aggravated by forceful grip, forearm pronation, and ulnar deviation.
Diagnosis
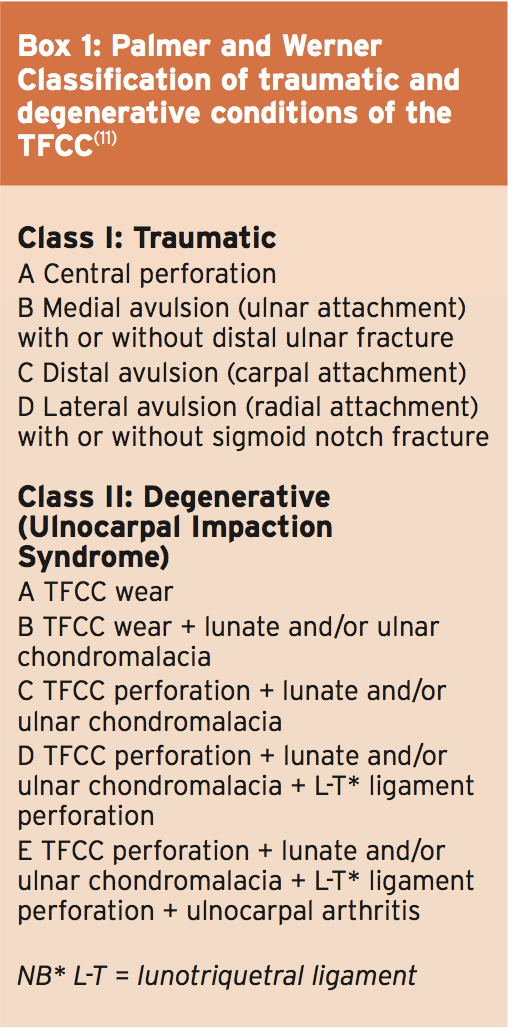
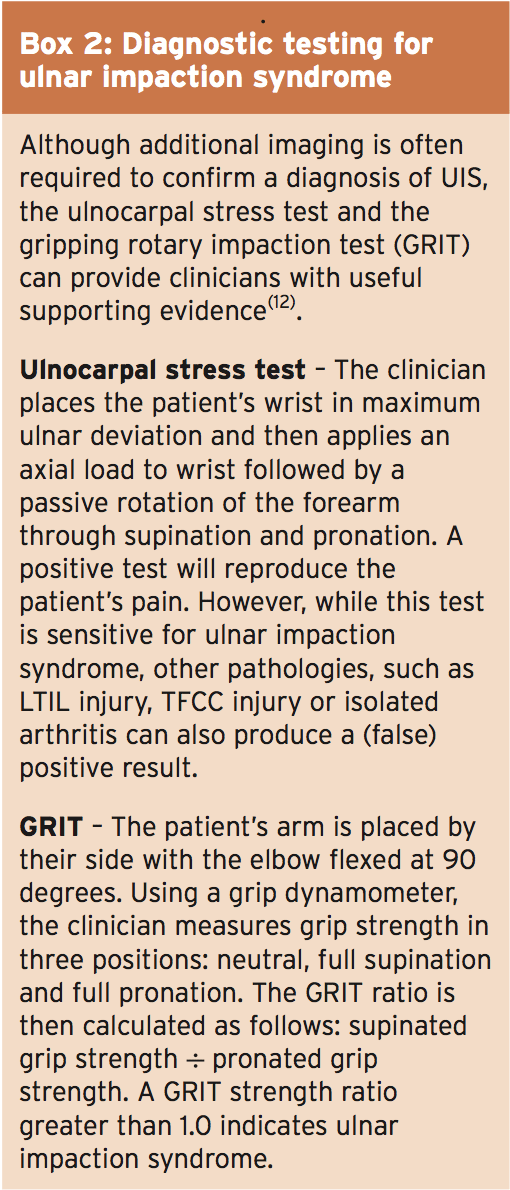
When attempting to make a diagnosis of UIS, a thorough wrist examination is necessary, together with a comprehensive patient history (as an example, has the individual suffered a radius fracture previously?) . Regrettably, however, there’s no single clinical test that can completely diagnose UIS, not least since most tests conducted in the clinic are inconclusive as to whether TFCC- related pain is acute or degenerative in nature (see Box 1). For this reason, diagnostic imaging (eg MRI) should be conducted to confirm the findings in the clinical examination. Having said that, the clinician can gain valuable supporting evidence from a comprehensive examination that includes the following:On palpation, is there:
- Tenderness just distal to ulnar head?
- Tenderness just volar to the ulnar styloid process?
- Positive ulnar variance, while stationary or dynamic?
- Painful ulnar deviation and forceful pronation?
- Decreased flexion, extension ulnar deviation?
- Reduced grip strength in comparison to the wrist if using dynamometer?
Is The Gripping Rotary Impaction Exam
(GRIT) positive? (see Box 2)The ulnocarpal stress test described in box 2 was initially introduced by Nakamura and his coworkers(13). In the writers’ unique study, 33 of 45 patients (73%) with favorable ulnocarpal stress test results revealed positive ulnar variance of 1mm or more about the wrist. In the 33 patients that had a positive ulnar variance, 19 (58%) were confirmed as suffering from course II TFCC lesions resulting from ulnocarpal impaction. The vast majority of those patients suffered a spontaneous onset of pain, and so were diagnosed with course IIB lesions involving TFCC wear with lunate and/or ulnar chondromalacia (see Box 1). Generally, a history of spontaneous ulnar sided wrist pain combined with testing should prompt the astute clinician to seek additional evaluation utilizing imaging.
Treatment Options
When treating athletes sooner is better; studies reveal that early diagnosis and intervention may significantly lessen the danger of long-term disability and injury progression(14,15). Treatment should be attempted before surgery and can include limiting movements such as pronation, gripping and ulnar deviation for 6-12 weeks or immobilization. After immobilzation/restriction, other conservative treatment choices include, non-steroidal anti- inflammatories (NSAIDs) and corticosteroid injections.However, while conservative therapies such as anti-inflammatories limiting range of motion or combined with immobilization may be effective for the overall populace, they are frequently insufficient for athletes because they do not deal with the fundamental biomechanical variables that predispose the athlete to UIS. Therefore, when conservative management fails to produce a substantial improvement, evidence indicates that surgery is indicated(16,17).
When surgery is required Athletes opt to postpone surgery before the season’s finish, permitting recovery from operation to take place. In terms of surgical possibilities, this is determined by the surgeon following screening that was comprehensive. These options may include:
- Ulnar shortening osteotomy — that the ulna is abbreviated by 2-3mm of shaft and fixated using a tubular or compression plate. This choice is indicated when there is ulnar wrist pain worsened a positive stress test by turning and ulnar deviation, and positive ulnar variance with or without changes.
- Arthroscopic wafer procedure — this process uses arthroscopy to debride the central triangular fibrocartilage tear, along with debridement of the distal pole of the ulna causing the impaction. The ulna’s debridement is performed to the degree at which the individual is neutral or slightly ulnar negative. The benefit of this process is that open operation is not mandatory, and recovery is faster. In the event the ulnar variance is greater than +4mm, then this choice isn’t suitable.
- Weeks 1 & 2 — control pain and swelling with ice/anti-inflammatory medication. Wearing a sugar-tong splint or long-arm cast to protect the surgical site while maintaining as much selection of movement (ROM) from rigid joints.
- Weeks 3 to 6 — Shield site and continue to maintain ROM in joints. Switch into a detachable splint or wrist cock-up brace. Try to boost wrist & knee ROM. Attend to scar management.
- Weeks 7 & 8 — Alter to removable splint worn in the nighttime. Progress to ROM present isometric elbow flexion/extension and supination/pronation and exercise for wrist & elbow.
- Weeks 9 onwards — continue with Stretching and mobilization. Introduce low-load resistance exercises to develop strength.
Summary
Although ulnar impaction syndrome is often congenital in its etiology, Athletic activity and years can combine to produce progressively more debilitating symptoms . For the clinician diagnosis is desirable but not always straightforward; even if scope of motion tests imply UIS, imaging will be asked to ascertain if intense or degenerative affects treatment options. Unless the UIS Is mild or the athlete is able to significantly modify his/her activity may be that treatment is unsuccessful and surgery is required. The choices will be different based on the person but in many cases- term results are favorable despite the requirement for recovery that is protracted and rehab after surgery.References
1. Hand Clinics. 2005: 21; 567 – 575
2. Clin Orthop Relat Res. 1984; 187: 26 – 35
3. J Hand Surg. 2013; 38(7): 746 – 750
4. Br J Hand Surg. 1998; 23(6):754 – 757
5. Magn Reso Imaging Clin N Am. 2004; 12: 281 – 299
6. J Hand Surg Am. 1993; 18(4): 713 – 716
7. Prim Care Clin Office Pract. 2013: 40; 431 – 451
8. J Med Sci.2001; 64: 81 – 91. J Ped Orthop. 1989; 9: 23 – 28
9. Hand Clin. 1990; 6: 493 – 505
10. Hand Clinics. 2005: 28; 307 – 321
11. J Can Chiropr Assoc 2014; 58(4)
12. J Hand Ther. 2001; 14(3): 173-179. J Hand Surg. 1997; 22B:719–723
13. Br J Hand Surg. 1991; 16: 84 – 88
14. Arthroscopic Rel Surg. 2004; 20(4): 392 – 401
15. Hand Clinics. 2005: 28; 307 – 321.2,6,8,31
16. J Hand Ther. 2001; 14(3): 173-179.
17. J Hand Surg. 2008; 33A: 1669-1679