Chiropractor, Dr. Alexander Jimenez explores some of the neurological and behavioral changes that pain can bring about, and the implications for clinicians with athletes in their care…
Pain following a sports injury is a common occurrence, and one that often leads to time off training. In this article, we will explore the consequences and effects of this pain in terms of tissue damage, immobilisation, fear avoidance, and ‘neural reorganisation’ in the brain – and what they mean for rehab guidelines in order to ensure full recovery and prevent future complications.
Pain can be described as an unpleasant sensory and emotional experience that occurs with either actual or potential tissue damage(1). Pain is the most common effect of sustaining a sports injury, and something that everyone will have experienced at some point.
Pain can be detected by the receptors at the local injury site called nociceptors.
These respond to thermal, mechanical and/ or chemical stimuli, and project a ‘pain message’ to the brain, where it is deciphered and a response is elicited. However, this process is distinct from neuralgia, which is a different type of pain that is experienced when there is actual nerve damage(2). Neuralgia-type pain can be felt throughout the length of the nerve – eg along the length of the whole leg.
Following an acute, local injury, the tissue damage that occurs elicits a cascade of effects, from the onset of inflammation, swelling, and the associated feeling of pain, as chemicals get released and the nociceptors respond to the influx of chemical and mechanical stimulation(2). These signals are transmitted to the brain where it is notified of this trauma, and a protective mechanism begins to occur in order to prevent further injury to the body. This protective mechanism can also make the pain appear far greater than the extent of the tissue damage.
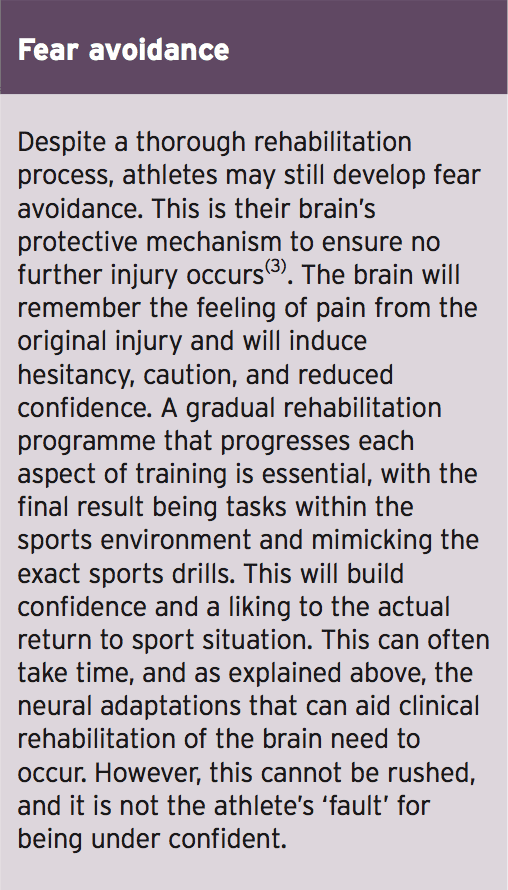
Following the correct treatment, these symptoms will all start to resolve. However, if symptoms of pain continue to persist beyond this acute phase and beyond the tissue healing, the pain is said to become chronic, and factors other than the tissue damage and initial injury come in to play. An athlete may then develop long-term pain with no physical cause. This can result in fear avoidance, anxiety, fatigue and muscle weakness(3).
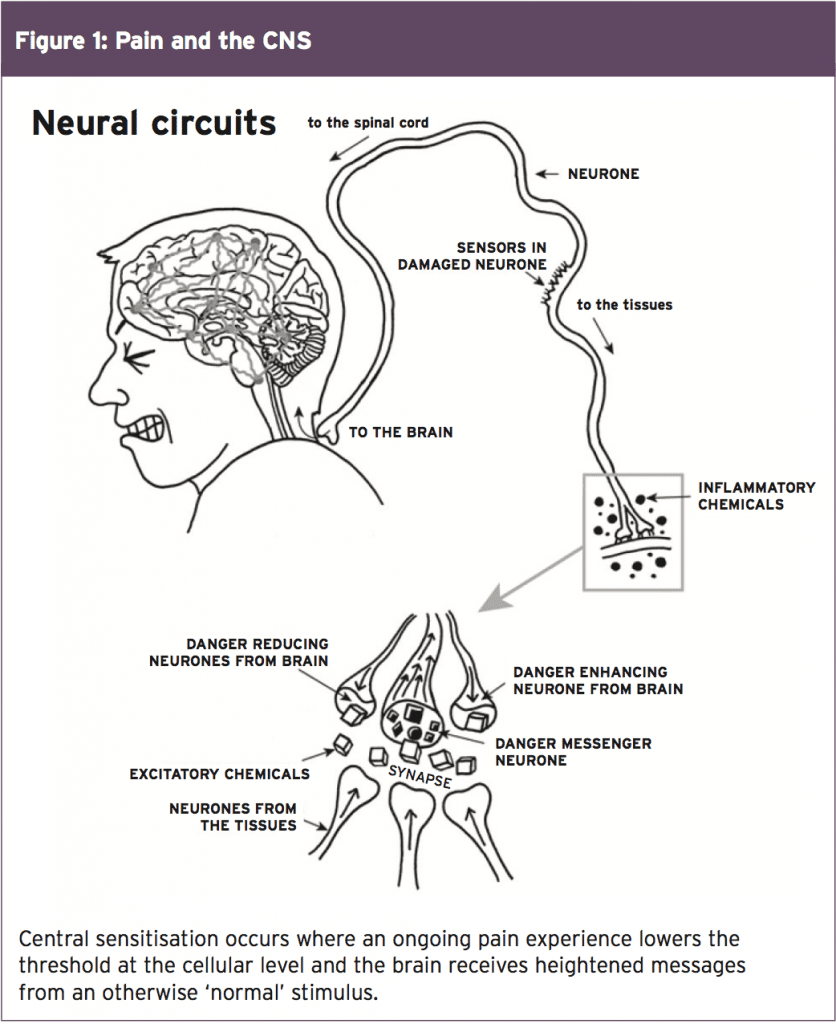
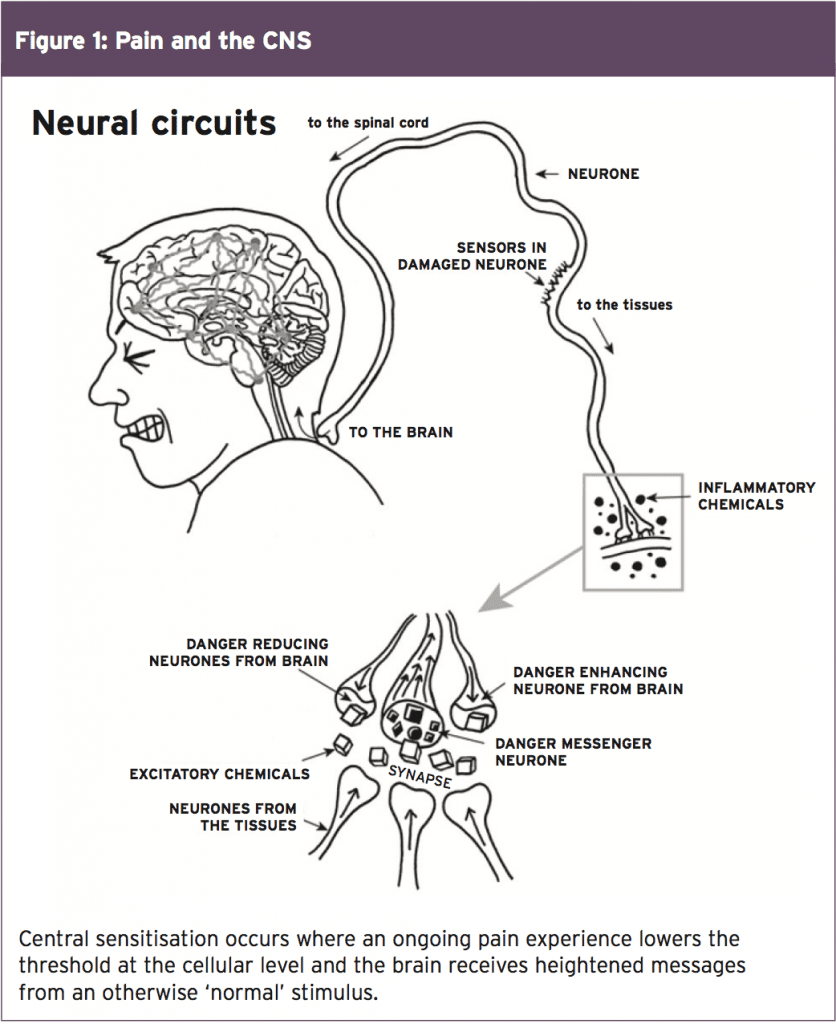
More specifically, athletes may experience allodynia (pain from a non-painful stimulus), or secondary hyperalgesia (an increased response to pain from a stimulus away from the area of injury)(4). These symptoms can lead to a phenomenon called ‘central sensitisation’, where the ongoing pain experience lowers the threshold at the cellular level and the brain receives heightened messages from a ‘normal’ stimulus (see Figure 1). This creates the feeling of tenderness and pain at areas away from the initial injury site.
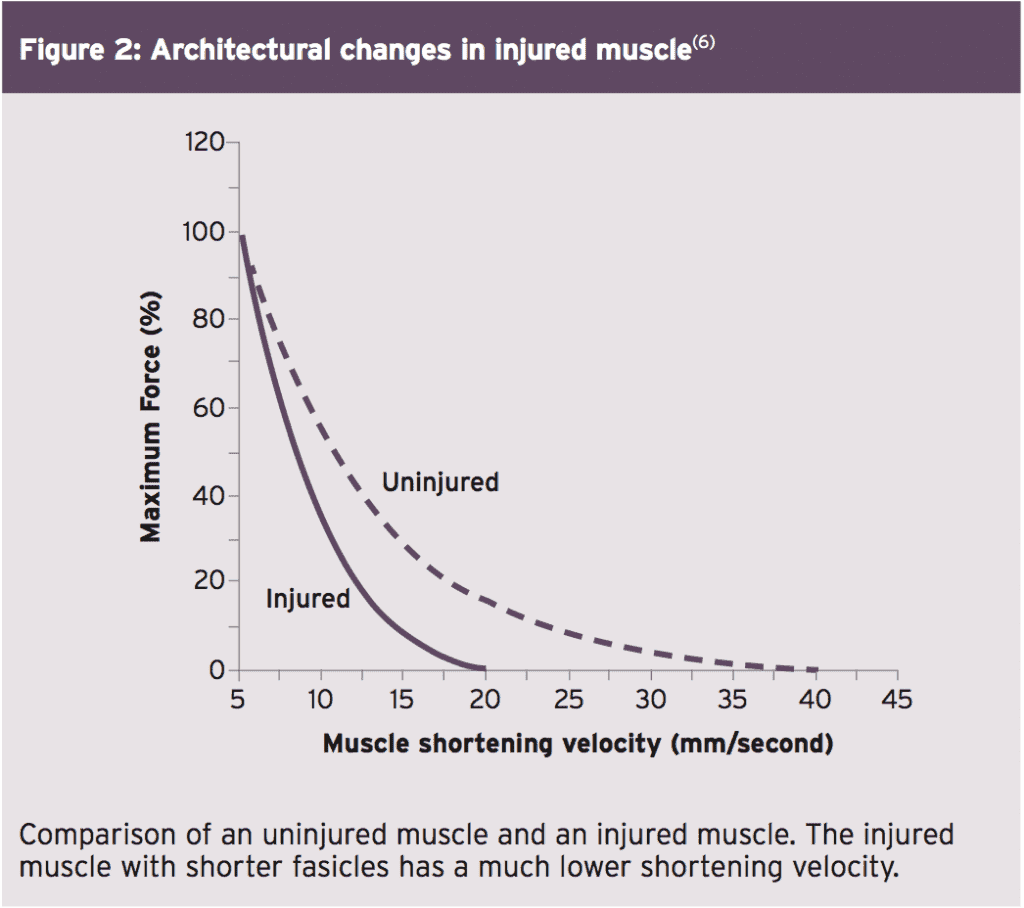
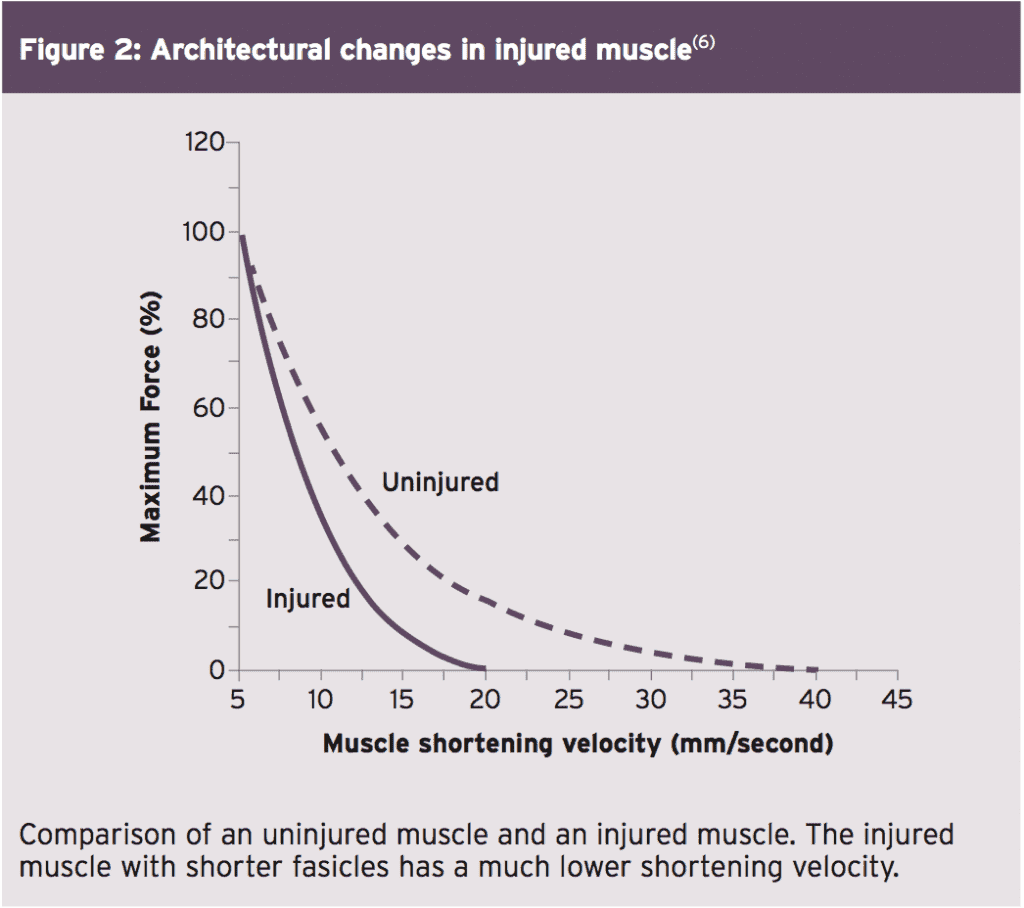
This has a significant impact on the function of the muscle post-injury and can alter the force-velocity and force-length relationships. For example, if the muscle fascicles are of a shorter length they have a smaller range to work through than normal, and therefore the force generation will also be smaller. As a result, the muscle will attempt to contract harder and potentially increase the risk of further tissue damage(6). Figure 2 shows how an injured muscle (which has shorter fascicles) will provide a slower maximal shortening velocity, ultimately affecting the muscle function due to the diminished output.
Scar tissue and tissue damage can also affect how the muscle fascicles function. These impairments to the connective tissue can impact the intramuscular nerve branches. These are the nerves that tell the muscles to contract and function. An injured muscle will therefore suffer from neuromuscular inhibition, where the nerves don’t fire as efficiently – with the result that the muscle will not respond as required. This sequence of events is difficult to break. In the early phases of rehabilitation the athlete often avoids exposing the injury to full range of movement (eg a full stretch of a muscle) because of pain and fear; the muscle therefore never receives the stimulus it requires (eg loading at these longer lengths) to adapt the structural change for healing(7).
In terms of treatment implications, evidence suggests that specific eccentric- loading exercises that isolate the injured muscle are appropriate(6). These are exercises that load the muscle in the lengthened position. Muscles should firstly be stretched and lengthened to eliminate pain and fear, followed by a gradual increase in eccentric loading.
This protocol should be commenced early in rehabilitation in order to prevent shortening of the fascicle lengths, and to tackle neuromuscular inhibition early on (before it worsens and the sensitivity induces reluctance to lengthen the muscle). If this protocol is not commenced early, protective shortening becomes a much harder phase to rehabilitate.
A group of brain cells that provide these outputs are called ‘neurotags’. Pain becomes a primary neurotag activator, and therefore makes these cells more likely to fire, causing the sensation of pain and sensitivity. Furthermore, any information received that could be perceived as a threat by the body becomes represented by secondary neurotags (eg competition, reduced movement etc) and this stimulates further protective mechanisms from the brain.
Graded motor imagery is the most researched area for treating these neural adaptations in response to prolonged pain. This is the process of graded exposure to motor tasks or skills to reinstate normal motor patterns within the brain(8). Neurotags loose strength and precision following injury, and continue to weaken the longer an athlete is out of practice. Therefore, early exposure to graded motor imagery is highly recommended to try prevent the decrease in neuronal strength. Exposure should also be given in tasks that might (incorrectly) signal danger to the body and tissues. This enables the neurotags to become accustomed to performing correctly under the kind of conditions that an athlete will encounter in competitive sport(3).
Graded motor imagery is the gold standard treatment choice. An accurate diagnosis and determination of stage of healing is vital, so that the correct pain mechanisms can be identified and treated accordingly. Behavioral education, a gradual increase in exercise load, specificity to the injury environment and return to play must all be considered.
References
1. IASP 1994. Ed 2. Classification of chronic pain. IASP Press
2. Sports Med. 2013; Sep: DOI 10.1007/s40279-013-0096-z
3. Br J Sports Med. 2016; 50:990-996
4. Hengeveld & Banks. 2014. Maitland’s Vertebral Manipulation. 8th Ed. Churchill Livingstone Elsevier. pg 125
5. J Physiol. 2007; 583(pt.2):1079-1091
6. Br J Sports Med. 2016; 50:1467-1472
7. J Electromyogr Kinesiol. 2013; 23:523-530
8. Neurorehabil Neural Repair. 2012; Jul-Aug: 26(6); 646-652
More specifically, athletes may experience allodynia (pain from a non-painful stimulus), or secondary hyperalgesia (an increased response to pain from a stimulus away from the area of injury)(4). These symptoms can lead to a phenomenon called ‘central sensitisation’, where the ongoing pain experience lowers the threshold at the cellular level and the brain receives heightened messages from a ‘normal’ stimulus (see Figure 1). This creates the feeling of tenderness and pain at areas away from the initial injury site.
The Implications Of Pain
The general effects of pain following injury are common knowledge to most. However, the architectural adaptations of the muscle and the neural adaptations of the brain are much more complicated and often under considered by clinicians. Here we consider the physical effects and the neural effects in turn.Physical Effects
Following injury, the onset of pain (and fear of what damage may have occurred) is likely to result in immobilization of the area until further information is known. When the injury is severe, immobilization can last for much longer to protect the region and allow healing. Unfortunately however, immobilization of muscle strains can result in a significant reduction in muscle fascicle length. A 6% reduction in muscle fascicle length within just 14 days has been reported(5).This has a significant impact on the function of the muscle post-injury and can alter the force-velocity and force-length relationships. For example, if the muscle fascicles are of a shorter length they have a smaller range to work through than normal, and therefore the force generation will also be smaller. As a result, the muscle will attempt to contract harder and potentially increase the risk of further tissue damage(6). Figure 2 shows how an injured muscle (which has shorter fascicles) will provide a slower maximal shortening velocity, ultimately affecting the muscle function due to the diminished output.
Scar tissue and tissue damage can also affect how the muscle fascicles function. These impairments to the connective tissue can impact the intramuscular nerve branches. These are the nerves that tell the muscles to contract and function. An injured muscle will therefore suffer from neuromuscular inhibition, where the nerves don’t fire as efficiently – with the result that the muscle will not respond as required. This sequence of events is difficult to break. In the early phases of rehabilitation the athlete often avoids exposing the injury to full range of movement (eg a full stretch of a muscle) because of pain and fear; the muscle therefore never receives the stimulus it requires (eg loading at these longer lengths) to adapt the structural change for healing(7).
In terms of treatment implications, evidence suggests that specific eccentric- loading exercises that isolate the injured muscle are appropriate(6). These are exercises that load the muscle in the lengthened position. Muscles should firstly be stretched and lengthened to eliminate pain and fear, followed by a gradual increase in eccentric loading.
This protocol should be commenced early in rehabilitation in order to prevent shortening of the fascicle lengths, and to tackle neuromuscular inhibition early on (before it worsens and the sensitivity induces reluctance to lengthen the muscle). If this protocol is not commenced early, protective shortening becomes a much harder phase to rehabilitate.
Neural Effects
During activity such as sport, the brain uses feedback from visual, spatial, proprioceptive, and tactile cues to identify body awareness and position within the environment. Using this information, it can then implement the movement planning, preparation, and execution of tasks. After injury, all of these mechanisms can be impaired. They must therefore be reinstated so that the brain can process them efficiently and effectively, to finely tune the precise movements and reactions required for a return to sport(3).A group of brain cells that provide these outputs are called ‘neurotags’. Pain becomes a primary neurotag activator, and therefore makes these cells more likely to fire, causing the sensation of pain and sensitivity. Furthermore, any information received that could be perceived as a threat by the body becomes represented by secondary neurotags (eg competition, reduced movement etc) and this stimulates further protective mechanisms from the brain.
Graded motor imagery is the most researched area for treating these neural adaptations in response to prolonged pain. This is the process of graded exposure to motor tasks or skills to reinstate normal motor patterns within the brain(8). Neurotags loose strength and precision following injury, and continue to weaken the longer an athlete is out of practice. Therefore, early exposure to graded motor imagery is highly recommended to try prevent the decrease in neuronal strength. Exposure should also be given in tasks that might (incorrectly) signal danger to the body and tissues. This enables the neurotags to become accustomed to performing correctly under the kind of conditions that an athlete will encounter in competitive sport(3).
By replicating the conditions experienced at the time of injury, this kind of exposure also help athletes to overcome the ‘fear’ of re-injury. For example, training drills can be performed around the same time of day, location and weather conditions as when the injury occurred, with similar background noise and distractions. This will encourage the athlete to experience the same mood and feelings at the time, and learn to cope with any particular stress or fatigue they were experiencing. Identifying one cue can initially commence this rehabilitation process. Then gradually exposing the athlete to more of these conditions will better prepare them for return to training environments.
Treatment Options
Given what we know about the physiology of pain after injury, what are the practical treatment implications for clinicians? Here are some pointers:- Diagnosis – An accurate diagnosis is essential to aiding the rehabilitation of any injury. The mechanism of the injury and time elapsed since the onset of injury will both provide an accurate picture of the physical, chemical, and neural implications on the injury.
- Education – Educating the athlete on their injury, what has happened and what rehabilitation will involve is absolutely paramount for a successful outcome and early return to sport. Athletes often get frustrated at lack of progress or unrealistic rehabilitation timeframes, therefore an understanding of why they have pain may ease this psychological barrier. If athletes can understand why the duration may be longer than desired and what is happening at the tissue and biochemical levels it can increase their commitment to rehab, and for longer. It can also help prevent unnecessary damage from trying to progress too early(3).
- Ice/heat – The use of ice and heat can greatly assist with the chemical processes occurring during injury. Typically, ice is used when there is suspected tissue inflammation, and heat when there is muscle spasm and tightened tissues. However, clinicians should always listen to the athlete and their response. If you are applying heat for the right reasons but they are complaining of worsening of their symptoms, then it is likely the C-fibres (fibres that detect sensation) are being stimulated, which is suggestive of underlying inflammation within the tissues(2).
- Exercise – Regular, controlled movement and exercise is imperative to preventing the shortening of the muscle fascicles and a detrimental effect on muscle function. This process also helps to minimize fear avoidance, promoting a positive outlook on rehabilitation.
In Summary
Pain is a sensory and emotional experience following actual or potential tissue damage. Pain triggers a cascade of events including physical changes such as immobilization and muscle shortening, and neural influences, where the muscle can be inhibited by pain and does not activate as required, or with delay. Behavioral changes including fear avoidance, reduced confidence, restriction on allowing the muscle to full length are also commonplace.Graded motor imagery is the gold standard treatment choice. An accurate diagnosis and determination of stage of healing is vital, so that the correct pain mechanisms can be identified and treated accordingly. Behavioral education, a gradual increase in exercise load, specificity to the injury environment and return to play must all be considered.
References
1. IASP 1994. Ed 2. Classification of chronic pain. IASP Press
2. Sports Med. 2013; Sep: DOI 10.1007/s40279-013-0096-z
3. Br J Sports Med. 2016; 50:990-996
4. Hengeveld & Banks. 2014. Maitland’s Vertebral Manipulation. 8th Ed. Churchill Livingstone Elsevier. pg 125
5. J Physiol. 2007; 583(pt.2):1079-1091
6. Br J Sports Med. 2016; 50:1467-1472
7. J Electromyogr Kinesiol. 2013; 23:523-530
8. Neurorehabil Neural Repair. 2012; Jul-Aug: 26(6); 646-652




