Medial tibial stress syndrome can be a persistent and debilitating condition in athletes. Chiropractor, Dr. Alexander Jimenez looks at the risk factors involved, the popular treatment options, and also considers the efficacy or otherwise of a novel approach based on fascial manipulation
Medial tibial stress syndrome (MTSS – commonly known as shin splints) is a frequent injury of the lower extremity and one of the most common causes of exertional leg pain in athletes and other active individuals. Studies suggest that the incidence of MTSS among physically active soldiers is 7.9%, while among athletes it varies between 4% and 35%(1,2). Although often not serious, it can be quite disabling, and progress to more serious complications if not treated properly. To further complicate matters, the rate of relapse in MTSS is high.
Causes of MTSS
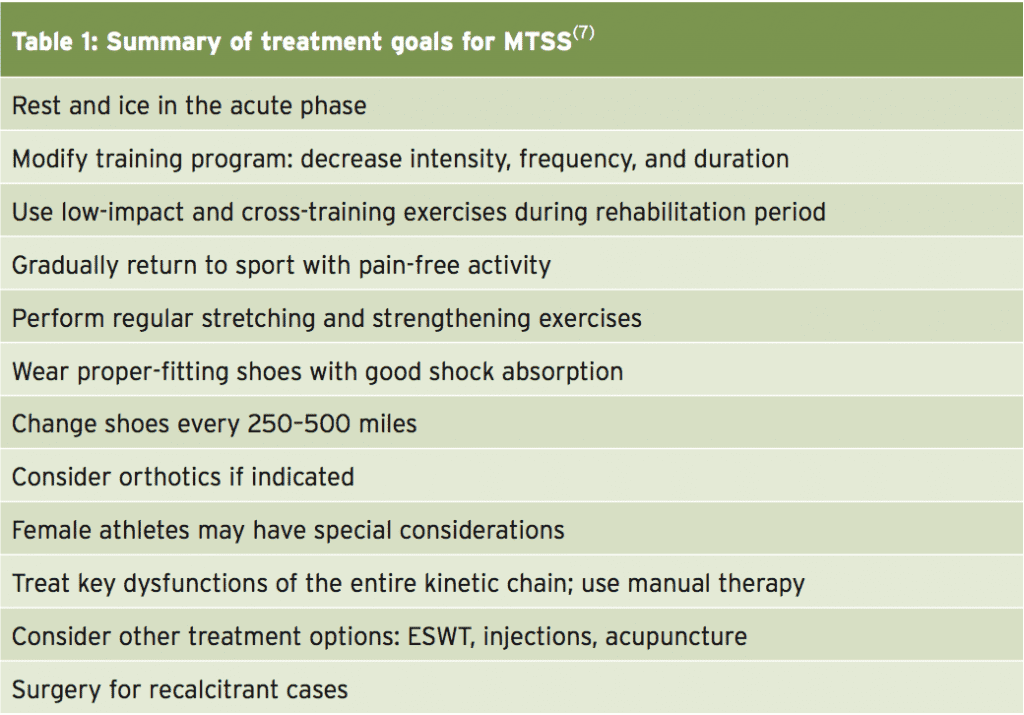
The precipitating factors leading to MTSS are thought to be multi-factorial, involving training errors and various biomechanical abnormalities (these factors are discussed at length by Alicia Filley in SIB issue 156). Many believe the main cause of MTSS involves underlying periostitis of the tibia due to tibial strain when under load. However, the associated lower leg anatomy makes this unlikely (see Figure 1). Also, other evidence indicates it is likely that a whole spectrum of tibial stress injuries are involved in MTSS, including tendinopathy, periostitis, periosteal remodeling, and stress reaction of the tibia(3-6).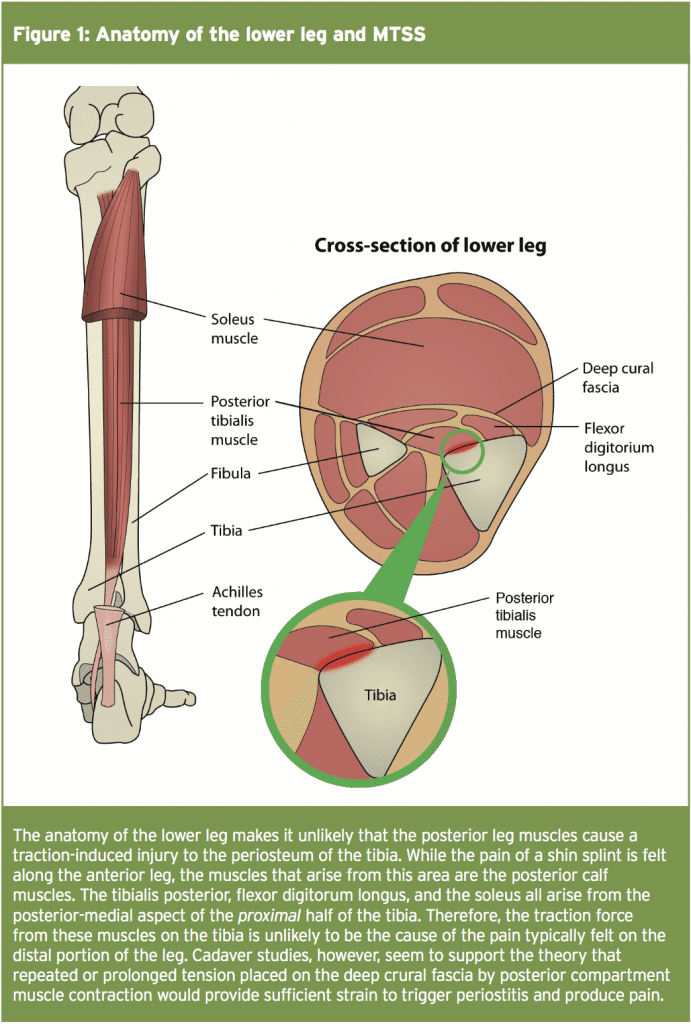
Dysfunction of the tibialis posterior, tibialis anterior, and soleus muscles are also commonly implicated(5,6). These various tibial stress injuries appear to be caused by alterations in tibial loading, as chronic, repetitive loads cause abnormal strain, bending of and micro-damage to the tibia. In other words, while MTSS is sometimes composed of different etiologies, MTSS and tibial stress fractures may be considered on a continuum of bone-stress reactions. One thing that is unarguable is that over the last few decades, comparatively few advances have been made in the treatment of MTSS. Current treatment options are mostly based on expert opinion and clinical experience rather than peer-reviewed comparative studies(7).
Assessment & Diagnosis
MTSS typically presents with vague, diffuse pain of the lower extremity, along the middle-distal tibia, and which is associated with exertion(13). In the early stages, pain is worse on commencing exercise and gradually subsides during training or shortly after the cessation of exercise. However, as the injury progresses, less and less activity is required to produce pain, and eventually it can occur even at rest.When faced with an athlete presenting with these symptoms, clinicians should obtain a comprehensive exercise history including:
- The athlete’s weekly exercise routine and total training volumes (eg total running mileage)
Exercise intensity/pace/loading - Footwear used
- Training terrain
Particular attention needs to be given to any of these factors that have changed radically over the past three months. This is because research suggests that MTSS is most likely to occur in athletes who have attempted to do ‘too much, too fast’(14,15).
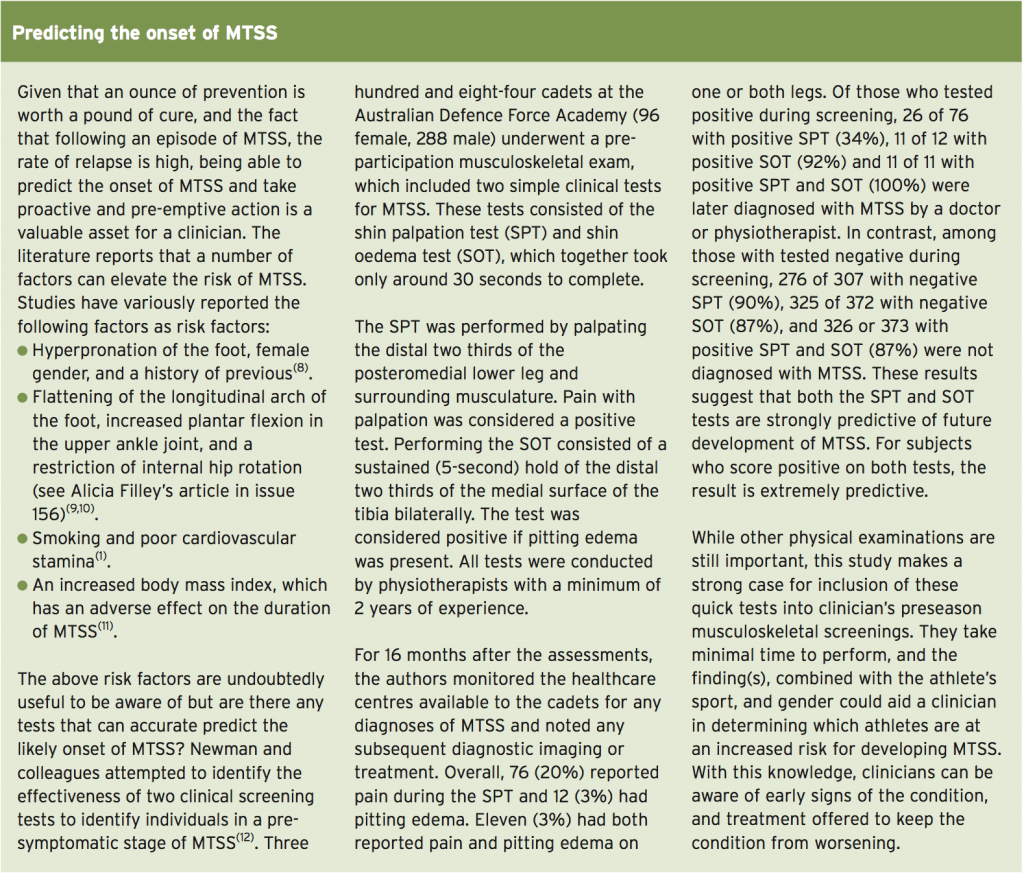
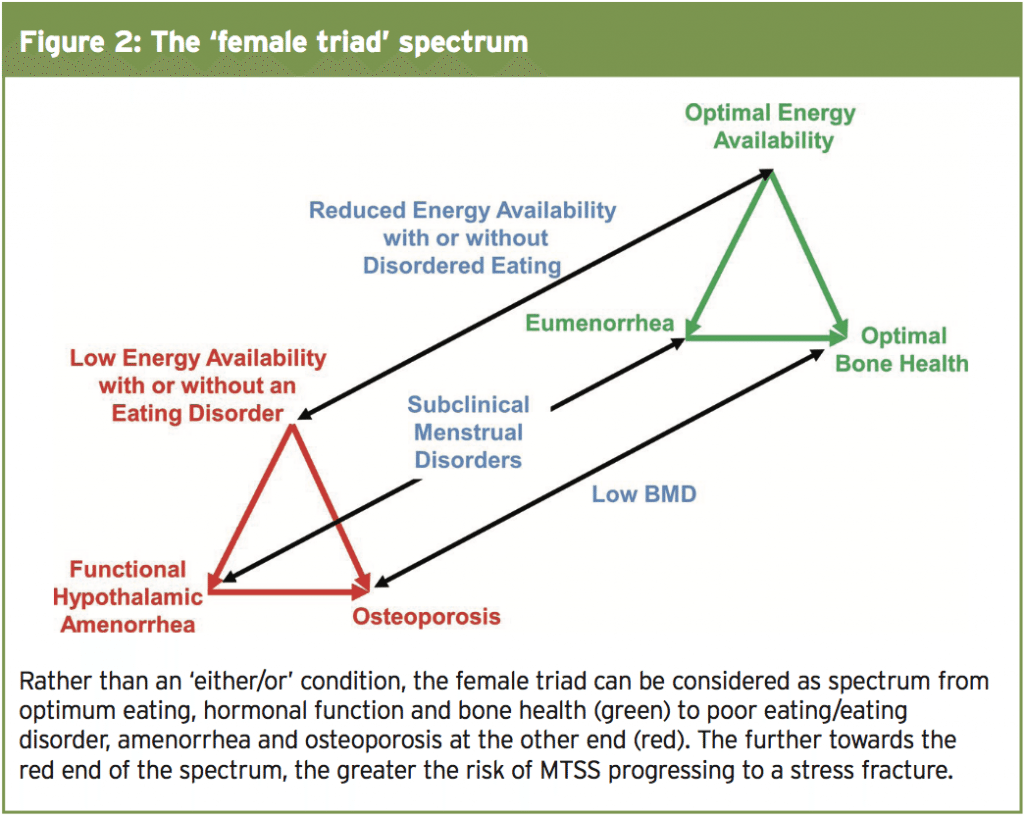
Common errors include a recent onset of rapidly increased activity, intensity, or duration(16). Running on hard or uneven surfaces is also a common risk factor and all risks are increased once weekly mileage exceeds around 20 miles per week(17). Clinicians should also be aware of the MTSS gender factor; studies indicate that the risk for progression to stress fractures is 1.5 to 3.5 times greater in females(17,18). This is especially relevant in females at risk of diminished bone density and osteoporosis – commonly observed is the ‘female athlete triad syndrome’ (osteoporosis, amenorrhea, and disordered eating – see Figure 2)(19).
However, because MTSS is often associated with biomechanical abnormalities of the lower extremity, clinicians should also evaluate their clients for possible knee abnormalities (especially genu varus or valgus), tibial torsion, femoral anteversion, foot arch abnormalities, or a leg-length discrepancy. Ankle movements and subtalar motion should also be evaluated. In addition, examining the athlete’s training shoes may reveal generally worn-out shoes or patterns consistent with a leg-length discrepancy or other biomechanical abnormalities. Abnormal gait patterns should be evaluated with the patient walking and running, either in the office hallway or on a treadmill.
A thorough history and physical examination are usually sufficient to make a diagnosis of MTSS. However, some patients may require further imaging or work-uptoruleoutstressfracturessuchof that of the tibia manifested by focal tenderness of the anterior tibia(17,20). Symptoms such as sensory or motor loss in association with exertional lower leg pain could indicate acute or chronic exertional compartment syndrome, which is one of the conditions most likely to be confused with MTSS. Peripheral vascular disease is another common cause of exertional leg pain in older and diabetic athletes. In this circumstances, further imaging, compartment pressure measurements, and vascular and nerve conduction studies may occasionally be required to reach the correct diagnosis(21).
Having said that, recent research suggests that MTSS can be diagnosed reliably using history and physical examination alone(22). In a study at multiple sports medicine sites in The Netherlands, athletes with non-traumatic lower leg pain were assessed for MTSS by two clinicians, who were each blinded to each others’ diagnoses. Forty-nine athletes participated of whom 46 completed both assessments. The prevalence of MTSS was among the athletes was 74%. Importantly, the percentage of agreement was very high at 96% and the ‘inter-rater reliability’ was almost perfect. Of note was that out of the 34 athletes diagnosed with MTSS, eleven were also found to have a concurrent lower leg injury, bearing out the findings discussed above.
Acute Phase
In the acute phase of MTSS, rest is recommended, with a complete or partial cessation of activity for 2-6 weeks depending on symptom severity(23). NSAIDs and paracetamol are often used for pain relief while ice application to the affected area directly after exercise for approximately 15-20 min is also commonly used in the acute period.
Given the undesirability of weeks of complete inactivity in athletes, other treatment modalities to speed healing have also been advocated in the acute phase. These include ultrasound, whirlpool baths, phonophoresis, augmented soft tissue mobilisation, electrical stimulation, and unweighted ambulation. However, while these are popular approaches among some clinicians, there’s little evidence in the literature that they offer tangible benefits over and above rest and ice(3,6,13-15).
Post-Acute Phase
Training modification – Once the initial symptoms have subsided, the goal is to enable the athlete to gradually return to training and competition without a relapse. Without doubt, the most important requirement is to modify the training regimen and address any biomechanical abnormalities. Research indicates that runners can continue to improve without cessation of activity so long as their weekly running distance, frequency, and intensity are reduced by at least 50%. In addition, they should eliminate running on hills and uneven or very firm surfaces, which increase loading on the tibia(3,13-15). A better option is train on a synthetic track or treadmill, both of which provide a uniform surface with more shock absorption. During the post-acute phase, athletes can benefit from cross training utilising other low-impact exercises such as pool running, swimming, elliptical trainers or stationary cycling. This is also the time for clinicians to work with athletes on proper technique and gait retraining, helping them to return to activity in a step-wise fashion. Over a period of weeks, training intensity and duration can be gradually increased and jumping exercises and hill running added as long as the athlete remains pain-free(3). However, athletes should scale back any exercises that exacerbate their symptoms or cause pain.
Footwear – Many studies report that appropriate footwear can reduce the incidence of MTSS(3,15, 23,24); athletes should therefore switch to shoes with sufficient shock-absorbing soles and insoles, in order to reduce forces through the lower limbs. Runners should also change running shoes every 250–500 miles, a distance at which most shoes lose up to 40% of their shock-absorbing capabilities and overall support(14,25). In addition, athletes with foot-related biomechanical problems may benefit from orthotics (13,14,16). Over-the- counter insoles may be sufficient to help with excessive foot pronation and low foot arch but problems caused by forefoot or rear foot abnormalities may benefit from custom orthotics(26).
Other possible treatments – A number of other treatment options that may be relevant in the post-acute phase of MTSS have been described in the literature. Extracorporeal shock wave therapy (ESWT) has been used to treat various tendinopathies of the lower extremity with varying degrees of success. However, there are no randomised control trials (RCTs) examining this approach in MTSS. Various injection methods, including cortisone, have successfully been used for decades to treat others injuries of the lower extremity(27-29). There are also newer methods, such as dry-needling, autologous blood injection, platelet-rich plasma, and prolotherapy, which seek to stimulate a local healing response in injured tissues. Once again however, no RCTs have been performed with these different injection techniques for MTSS. The same is true for acupuncture. This is not to say that clinicians should rule out experimentation with these techniques – only that the evidence they are of value is lacking.
Some researchers have postulated that the fascia plays an important role in pathophysiology of MTSS. Bouché and Johnson have hypothesised that with contraction of the deep leg flexors, tension would be imparted to the tibial fascial attachment at the medial tibial crest and that circumferential straps would dampen tension directed to the medial tibial crest(33). Meanwhile, Stickley et al. Have described the tibial attachments of the deep crural fascia and concluded that there is deep crural fascia involvement in the aetiology of MTSS(34).
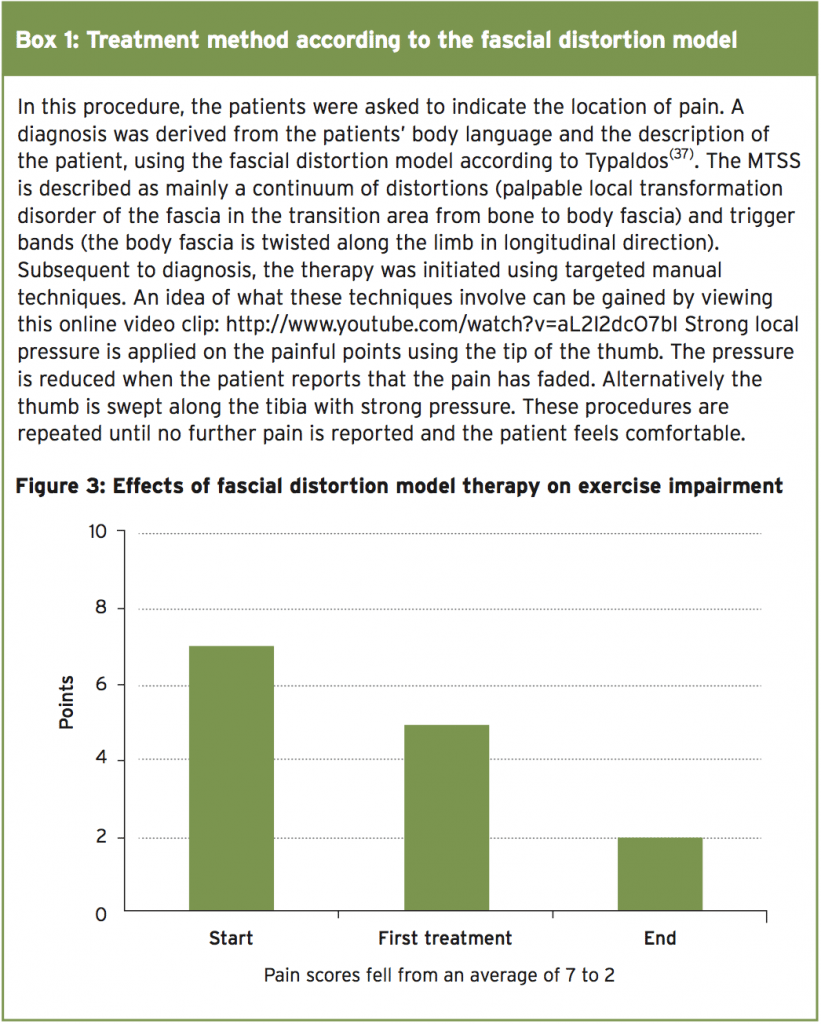
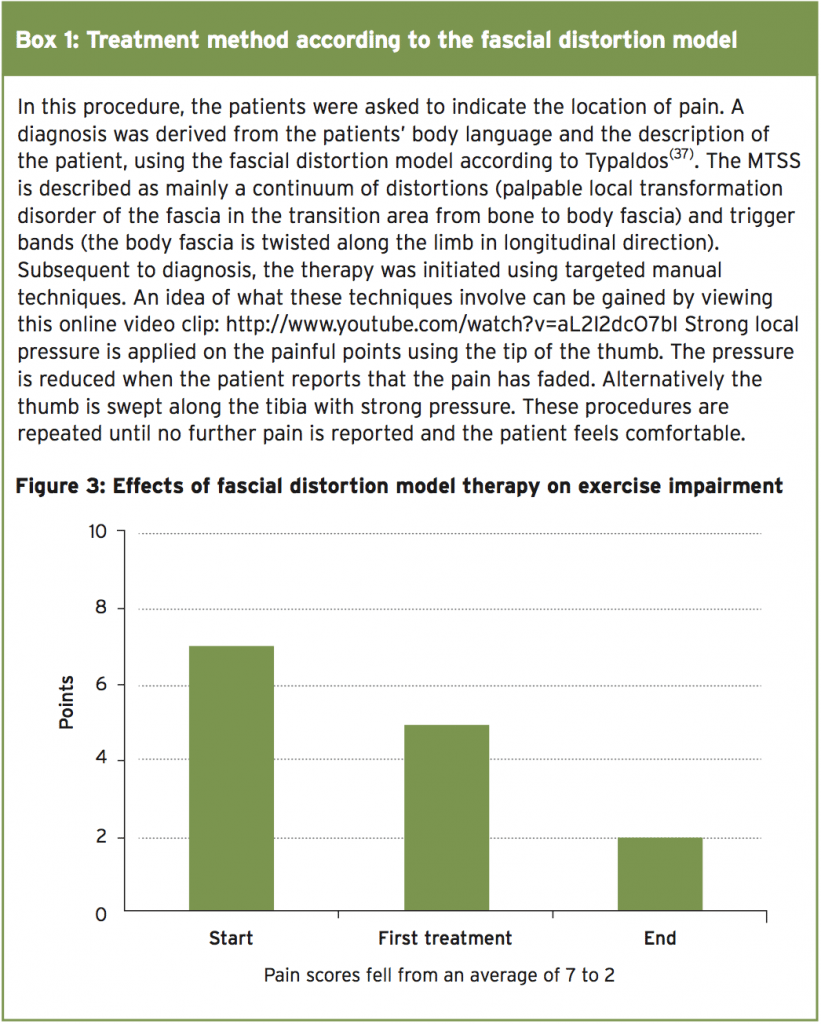
Before and after the intervention period, the patients performed running and jumping tests and a visual analogue scale (VAS) was used for the quantification of pain. Scores were also given to rate the maximum painless exercise tolerance of the patients. Following initial testing, treatment of the crural fascia was performed using the techniques described in box 1. The therapy was continued until full exercise tolerance or painlessness was reached. The main finding was that a significant reduction of the VAS pain score (from 5.2 to 1.1) was achieved in a relatively short time span (the duration of treatment was just 6.3 days on average). Also, the impairment of exercise tolerance following therapy was reduced from 7 to 2 points (see Figure 3).
The results of this clinical study suggest that the treatment method according to the fascial distortion model could be an effective option to relieve patients of pain and restore their exercise tolerance. The duration of this treatment was significantly shorter than the therapy periods indicated in the literature for shock wave therapy and physiotherapy(38,39). The drawback for the clinician however is that this method is time consuming. In severe cases, a complete initial treatment can take up to one hour for each lower leg (although the time expenditure will decrease in the subsequent treatment sessions). Moreover, the method is very painful for the patient, and the patient must be informed of this prior to treatment in order to improve the therapy tolerance.
Common errors include a recent onset of rapidly increased activity, intensity, or duration(16). Running on hard or uneven surfaces is also a common risk factor and all risks are increased once weekly mileage exceeds around 20 miles per week(17). Clinicians should also be aware of the MTSS gender factor; studies indicate that the risk for progression to stress fractures is 1.5 to 3.5 times greater in females(17,18). This is especially relevant in females at risk of diminished bone density and osteoporosis – commonly observed is the ‘female athlete triad syndrome’ (osteoporosis, amenorrhea, and disordered eating – see Figure 2)(19).
Physical Examination & Differential Diagnosis
Clinicians should complete a thorough musculoskeletal examination of the patient, focussing on the lower extremity. Typically, the medial ridge of the tibia (origin of the tibialis posterior and soleus muscles) will be tender to palpation, especially at the distal and middle tibial regions. The anterior tibia, however, is usually non-tender. Neurovascular symptoms are usually absent(13).However, because MTSS is often associated with biomechanical abnormalities of the lower extremity, clinicians should also evaluate their clients for possible knee abnormalities (especially genu varus or valgus), tibial torsion, femoral anteversion, foot arch abnormalities, or a leg-length discrepancy. Ankle movements and subtalar motion should also be evaluated. In addition, examining the athlete’s training shoes may reveal generally worn-out shoes or patterns consistent with a leg-length discrepancy or other biomechanical abnormalities. Abnormal gait patterns should be evaluated with the patient walking and running, either in the office hallway or on a treadmill.
A thorough history and physical examination are usually sufficient to make a diagnosis of MTSS. However, some patients may require further imaging or work-uptoruleoutstressfracturessuchof that of the tibia manifested by focal tenderness of the anterior tibia(17,20). Symptoms such as sensory or motor loss in association with exertional lower leg pain could indicate acute or chronic exertional compartment syndrome, which is one of the conditions most likely to be confused with MTSS. Peripheral vascular disease is another common cause of exertional leg pain in older and diabetic athletes. In this circumstances, further imaging, compartment pressure measurements, and vascular and nerve conduction studies may occasionally be required to reach the correct diagnosis(21).
Having said that, recent research suggests that MTSS can be diagnosed reliably using history and physical examination alone(22). In a study at multiple sports medicine sites in The Netherlands, athletes with non-traumatic lower leg pain were assessed for MTSS by two clinicians, who were each blinded to each others’ diagnoses. Forty-nine athletes participated of whom 46 completed both assessments. The prevalence of MTSS was among the athletes was 74%. Importantly, the percentage of agreement was very high at 96% and the ‘inter-rater reliability’ was almost perfect. Of note was that out of the 34 athletes diagnosed with MTSS, eleven were also found to have a concurrent lower leg injury, bearing out the findings discussed above.
Treatment Options For MTSS
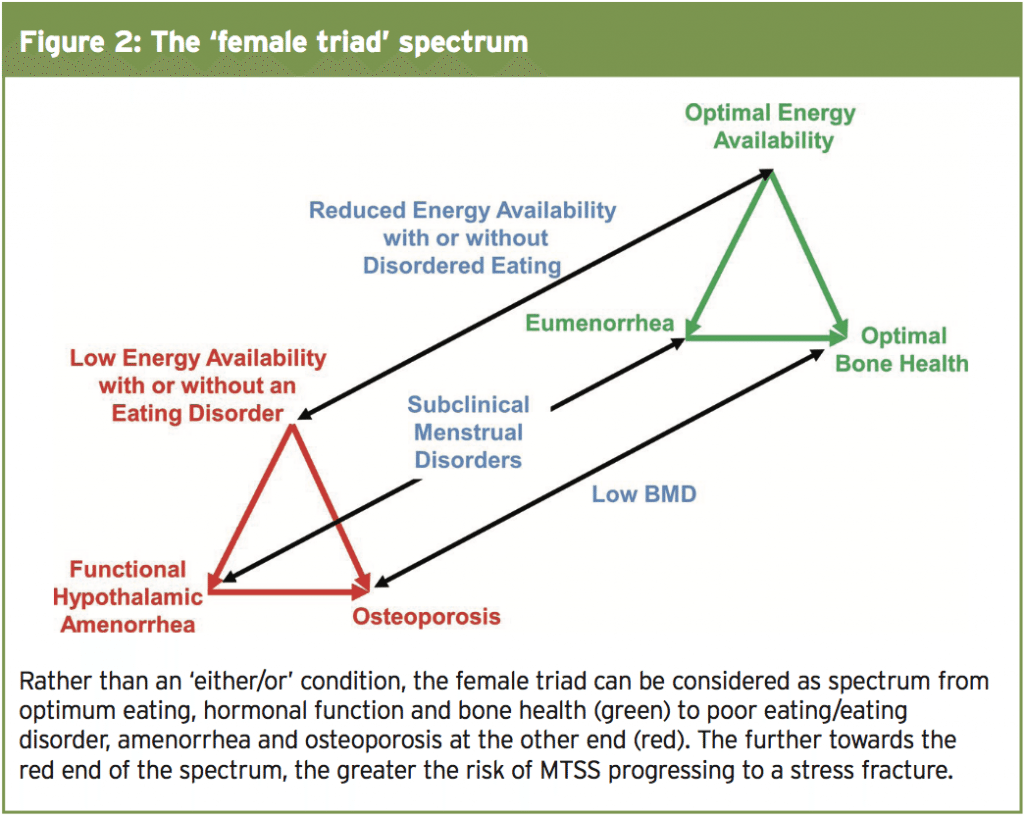
There are a number of conservative treatment options for MTSS. As we will see shortly however, some have been shown to be more effective than others. An excellent and detailed description of these approaches is described by Galbraith and Laverlee(7). In their paper, a brief summary of the conventional treatment pathway is also described (shown here in Table 1).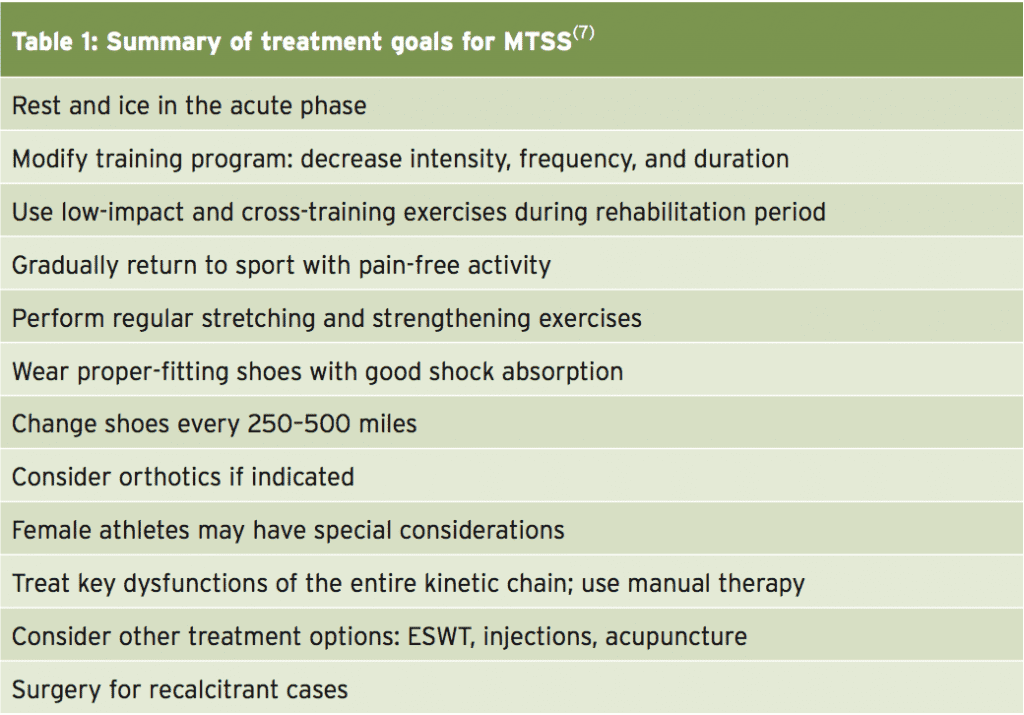
Acute Phase
In the acute phase of MTSS, rest is recommended, with a complete or partial cessation of activity for 2-6 weeks depending on symptom severity(23). NSAIDs and paracetamol are often used for pain relief while ice application to the affected area directly after exercise for approximately 15-20 min is also commonly used in the acute period.
Given the undesirability of weeks of complete inactivity in athletes, other treatment modalities to speed healing have also been advocated in the acute phase. These include ultrasound, whirlpool baths, phonophoresis, augmented soft tissue mobilisation, electrical stimulation, and unweighted ambulation. However, while these are popular approaches among some clinicians, there’s little evidence in the literature that they offer tangible benefits over and above rest and ice(3,6,13-15).
Post-Acute Phase
Training modification – Once the initial symptoms have subsided, the goal is to enable the athlete to gradually return to training and competition without a relapse. Without doubt, the most important requirement is to modify the training regimen and address any biomechanical abnormalities. Research indicates that runners can continue to improve without cessation of activity so long as their weekly running distance, frequency, and intensity are reduced by at least 50%. In addition, they should eliminate running on hills and uneven or very firm surfaces, which increase loading on the tibia(3,13-15). A better option is train on a synthetic track or treadmill, both of which provide a uniform surface with more shock absorption. During the post-acute phase, athletes can benefit from cross training utilising other low-impact exercises such as pool running, swimming, elliptical trainers or stationary cycling. This is also the time for clinicians to work with athletes on proper technique and gait retraining, helping them to return to activity in a step-wise fashion. Over a period of weeks, training intensity and duration can be gradually increased and jumping exercises and hill running added as long as the athlete remains pain-free(3). However, athletes should scale back any exercises that exacerbate their symptoms or cause pain.
Footwear – Many studies report that appropriate footwear can reduce the incidence of MTSS(3,15, 23,24); athletes should therefore switch to shoes with sufficient shock-absorbing soles and insoles, in order to reduce forces through the lower limbs. Runners should also change running shoes every 250–500 miles, a distance at which most shoes lose up to 40% of their shock-absorbing capabilities and overall support(14,25). In addition, athletes with foot-related biomechanical problems may benefit from orthotics (13,14,16). Over-the- counter insoles may be sufficient to help with excessive foot pronation and low foot arch but problems caused by forefoot or rear foot abnormalities may benefit from custom orthotics(26).
Other possible treatments – A number of other treatment options that may be relevant in the post-acute phase of MTSS have been described in the literature. Extracorporeal shock wave therapy (ESWT) has been used to treat various tendinopathies of the lower extremity with varying degrees of success. However, there are no randomised control trials (RCTs) examining this approach in MTSS. Various injection methods, including cortisone, have successfully been used for decades to treat others injuries of the lower extremity(27-29). There are also newer methods, such as dry-needling, autologous blood injection, platelet-rich plasma, and prolotherapy, which seek to stimulate a local healing response in injured tissues. Once again however, no RCTs have been performed with these different injection techniques for MTSS. The same is true for acupuncture. This is not to say that clinicians should rule out experimentation with these techniques – only that the evidence they are of value is lacking.
Fascial Distortion & MTSS
Manual therapy techniques such as osteopathic manipulation, stretching and massage have been commonly used to treat lower-extremity injuries with the benefit of improved pain and function(30-32). However, there is a paucity of properly controlled scientific trials into the role of manual therapy in treating specifically MTSS.Some researchers have postulated that the fascia plays an important role in pathophysiology of MTSS. Bouché and Johnson have hypothesised that with contraction of the deep leg flexors, tension would be imparted to the tibial fascial attachment at the medial tibial crest and that circumferential straps would dampen tension directed to the medial tibial crest(33). Meanwhile, Stickley et al. Have described the tibial attachments of the deep crural fascia and concluded that there is deep crural fascia involvement in the aetiology of MTSS(34).
The treatment of fascial distortions is also based on targeted manual therapy techniques, which has led some researchers to suggest that this approach could be effective in MTSS. Therapeutic success using this approach has already been described for shoulder pain, in particular for the management of frozen shoulder, where improvements in function and pain sensation were quickly achieved and superior to conventional physiotherapy(35,36).
New Research
A recent study has suggested that a treatment therapy based on the fascial distortion model could be a useful adjunct for clinicians seeking to hasten the recovery of athletes suffering from MTSS. The 32 participants in the study were soldiers who had been diagnosed with MTSS, because they showed the typical symptoms of pain following exercise as well as tenderness of the anterior or posterior medial and lateral anterior surfaces of the tibia. In some cases, the symptoms were acute, while in some patients the symptoms had been present for several years.Before and after the intervention period, the patients performed running and jumping tests and a visual analogue scale (VAS) was used for the quantification of pain. Scores were also given to rate the maximum painless exercise tolerance of the patients. Following initial testing, treatment of the crural fascia was performed using the techniques described in box 1. The therapy was continued until full exercise tolerance or painlessness was reached. The main finding was that a significant reduction of the VAS pain score (from 5.2 to 1.1) was achieved in a relatively short time span (the duration of treatment was just 6.3 days on average). Also, the impairment of exercise tolerance following therapy was reduced from 7 to 2 points (see Figure 3).
The results of this clinical study suggest that the treatment method according to the fascial distortion model could be an effective option to relieve patients of pain and restore their exercise tolerance. The duration of this treatment was significantly shorter than the therapy periods indicated in the literature for shock wave therapy and physiotherapy(38,39). The drawback for the clinician however is that this method is time consuming. In severe cases, a complete initial treatment can take up to one hour for each lower leg (although the time expenditure will decrease in the subsequent treatment sessions). Moreover, the method is very painful for the patient, and the patient must be informed of this prior to treatment in order to improve the therapy tolerance.
Furthermore, this study only demonstrated that exercise tolerance in MTSS can be restored within a short time by targeted manual intervention; there was no long-term follow up. Moreover, there was no direct comparison with alternative treatment options – this would be desirable to prove that therapy based on fascial distortion is superior to other therapeutic approaches. Despite these caveats however, therapy according to the fascial distortion model has proved to be superior to other physiotherapy methods in the management of shoulder pain syndromes(35,36), which suggests that this approach could be another weapon in the clinician’s armoury when seeking a rapid resolution of MTSS in athletes.
References
References
1. Gait & Posture. 2011;33(3):361–365
2. Clinics in Sports Medicine. 2012;31(2):273–
290
3. Sports Med. 1998;26(4):265–279
4. Radiology. 1997;204:177–180
5. Sports Med. 1986;3(6):436–446
6. Am J Sports Med. 1995;23:427–481
7. Curr Rev Musculoskelet Med. 2009 Sep; 2(3):
127–133
8. MTSS Clin Sports Med. 2012 Apr;31(2):273-90
9. Journal of Foot and Ankle Surgery.
2008;47(2):89–95
10. Scandinavian Journal of Medicine and
Science in Sports. 2012;22(1):34–39
11. Journal of Orthopaedic and Sports Physical
Therapy. 2007;37(2):40–47
12. Br J Sports Med. 2012 Sep;46(12):861-4
13. Med Sci Sports Exerc. 2000;32(3 suppl):S27–
S33
14. Sports Med. 1996;21:49–72
15. Clin Sports Med. 2004;23:55–81
16. Phys Med Rehabil Clin N Am. 2006;17(3):537–
552
17. Phys Med Rehabil Clin N Am. 2007;18(3):401–
416
18. J Sports Med Phys Fitness. 1990;30(3):307–
315
19. Am J Sports Med. 2004;32(3):772–780
20. Am J Sports Med. 1978;6(6):391–396
21. Phys Sportsmed. 2001;29(6):35–50
22. Br J Sports Med. 2017 Feb 8. pii:
bjsports-2016-097037
23. Phys Sportsmed. 2002;30(6):29–361
24. Med Sci Sports Exerc. 2002;34(1):32–40
25. Am J Sports Med. 1985;13:248–253
26. Med Sci Sports Exerc. 1995;27:800–804
27. Br J Sports Med. 2007;41(8):518–522
28. Am J Sports Med. 2006;34(11):1738–1746
29. Br J Sports Med. 2002;36(3):173–177
30. J Am Osteopath Assoc. 2005;105(12):563–
567
31. J Am Osteopath Assoc. 2006;106(9):537–
545
32. J Am Chiropr Assoc. 2004;41(9):32–42
33. Journal Am Podiatric Med Assoc.
2007;97(1):31–36
34. Med Sci Sports Exercise. 2009;41(11):1991–
1996
35. Zeitschrift fur Orthopadie und
Unfallchirurgie. 2012;150(4):420–427
36. Stein C. Untersuchung der Wirksamkeit
einer manuellen Behandlungstechnik nach dem
Faszien-Distorsions-Modell bei schmerzhaft
eingeschränkter Schulterbeweglichkeit – Eine
explorativ-prospektive, randomisierte und
kontrollierte klinische Studie. Medizinische
Hochschule Hannover; 2008
37. European Fascial Distortion Model
Association . Das Fasziendistorsionsmodell
(FDM) nach Stephan Typaldos D.O. Die TypaldosMethode.
1st. Bramsche, Germany: Rasch
Druckerei; 2012
38. Clinics in Sports Medicine. 2012;31(2):273–
290
39. British Journal of Sports Medicine.
2012;46(4):253–257
2. Clinics in Sports Medicine. 2012;31(2):273–
290
3. Sports Med. 1998;26(4):265–279
4. Radiology. 1997;204:177–180
5. Sports Med. 1986;3(6):436–446
6. Am J Sports Med. 1995;23:427–481
7. Curr Rev Musculoskelet Med. 2009 Sep; 2(3):
127–133
8. MTSS Clin Sports Med. 2012 Apr;31(2):273-90
9. Journal of Foot and Ankle Surgery.
2008;47(2):89–95
10. Scandinavian Journal of Medicine and
Science in Sports. 2012;22(1):34–39
11. Journal of Orthopaedic and Sports Physical
Therapy. 2007;37(2):40–47
12. Br J Sports Med. 2012 Sep;46(12):861-4
13. Med Sci Sports Exerc. 2000;32(3 suppl):S27–
S33
14. Sports Med. 1996;21:49–72
15. Clin Sports Med. 2004;23:55–81
16. Phys Med Rehabil Clin N Am. 2006;17(3):537–
552
17. Phys Med Rehabil Clin N Am. 2007;18(3):401–
416
18. J Sports Med Phys Fitness. 1990;30(3):307–
315
19. Am J Sports Med. 2004;32(3):772–780
20. Am J Sports Med. 1978;6(6):391–396
21. Phys Sportsmed. 2001;29(6):35–50
22. Br J Sports Med. 2017 Feb 8. pii:
bjsports-2016-097037
23. Phys Sportsmed. 2002;30(6):29–361
24. Med Sci Sports Exerc. 2002;34(1):32–40
25. Am J Sports Med. 1985;13:248–253
26. Med Sci Sports Exerc. 1995;27:800–804
27. Br J Sports Med. 2007;41(8):518–522
28. Am J Sports Med. 2006;34(11):1738–1746
29. Br J Sports Med. 2002;36(3):173–177
30. J Am Osteopath Assoc. 2005;105(12):563–
567
31. J Am Osteopath Assoc. 2006;106(9):537–
545
32. J Am Chiropr Assoc. 2004;41(9):32–42
33. Journal Am Podiatric Med Assoc.
2007;97(1):31–36
34. Med Sci Sports Exercise. 2009;41(11):1991–
1996
35. Zeitschrift fur Orthopadie und
Unfallchirurgie. 2012;150(4):420–427
36. Stein C. Untersuchung der Wirksamkeit
einer manuellen Behandlungstechnik nach dem
Faszien-Distorsions-Modell bei schmerzhaft
eingeschränkter Schulterbeweglichkeit – Eine
explorativ-prospektive, randomisierte und
kontrollierte klinische Studie. Medizinische
Hochschule Hannover; 2008
37. European Fascial Distortion Model
Association . Das Fasziendistorsionsmodell
(FDM) nach Stephan Typaldos D.O. Die TypaldosMethode.
1st. Bramsche, Germany: Rasch
Druckerei; 2012
38. Clinics in Sports Medicine. 2012;31(2):273–
290
39. British Journal of Sports Medicine.
2012;46(4):253–257




